Have you been suffering from sharp pains or burning in your abdomen that just won’t go away? Is this pain making it difficult to complete your daily activities? You may have caught an H. Pylori infection. Healing H. pylori requires guidance from a skilled healthcare practitioner. So don’t worry, we will have you feeling better in no time!
What is Helicobacter pylori?
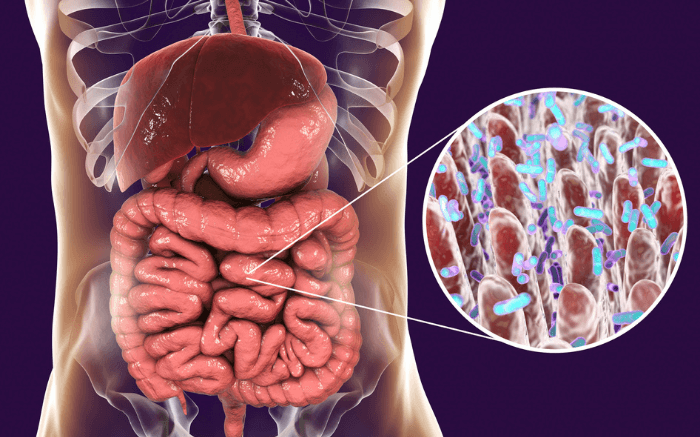
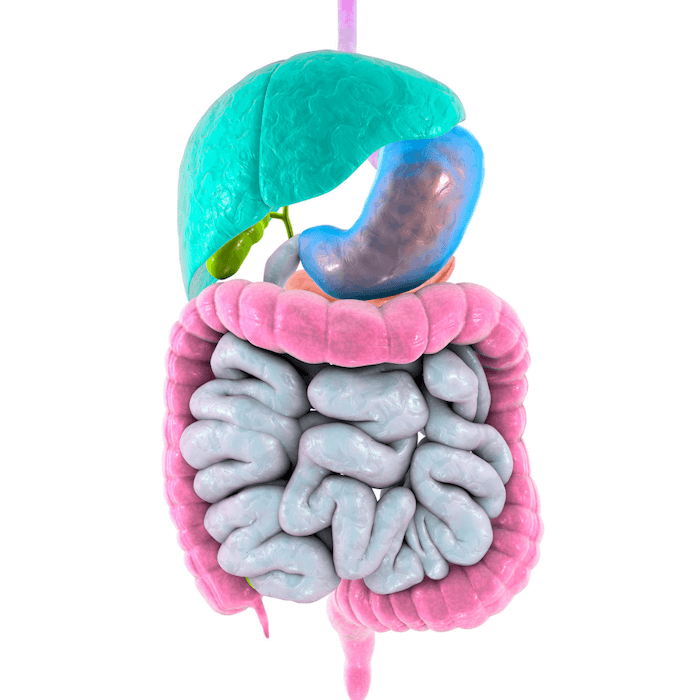
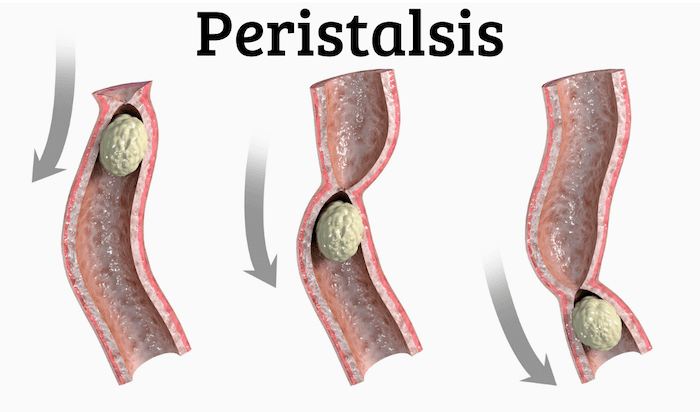
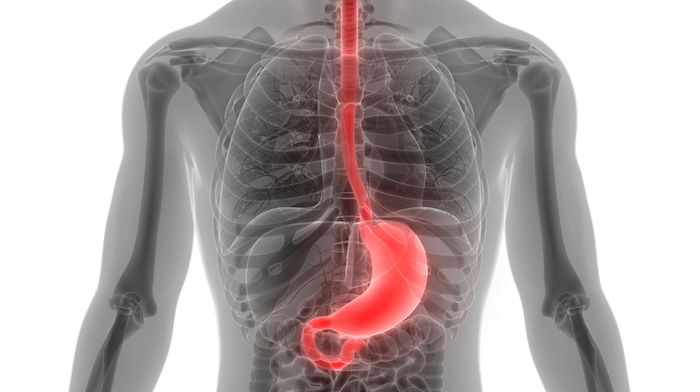
Helicobacter pylori is a type of bacteria that lives within the stomach. It releases toxins into the lining of the stomach, going through several layers of mucus and stomach tissue. This causes damage to the stomach lining and reduces stomach acid production.
Stomach acid is necessary to break down proteins, and low stomach acid means food is not digested as fully or efficiently as it would under normal conditions. This affects amino acid absorption, meaning the body is not able to absorb all the nutrients from your food, impacting every cell in the body.
By limiting amino acid absorption, an H. pylori infection can impact the production of:
- Antibodies/Immunoglobulins (responsible for fighting against infection)
- All enzymes (responsible for energy production and other bodily processes)
- Thyroid hormones, insulin, follicle-stimulating hormone, and all other amino acid-based hormones
- Hemoglobin and ferritin (store critical proteins transported to all cells and tissues)
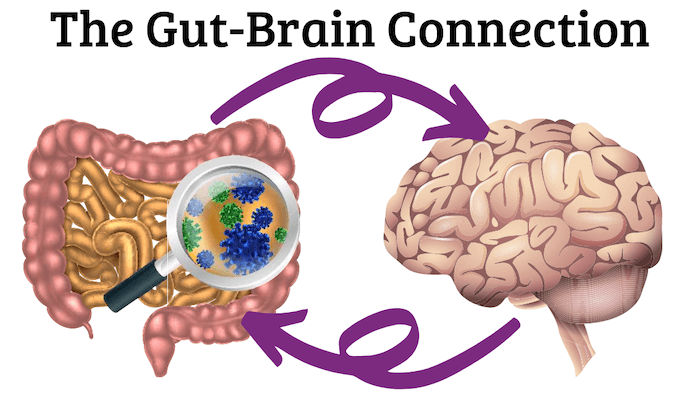
- Neurotransmitters
The body tries to fight against these toxins by using inflammation as a natural defense. Inflammation is a common response to any type of trauma to the body because it wakes up the immune system and encourages phagocytes, your own personal fighter cells, to come to the area.
The resulting inflammation may be responsible for the pain that you may be feeling from the infection. Unfortunately, the H. pylori bacterium has evolved to be prepared for the inflammation response and is immune to it, allowing for the infection to persist if not treated properly.
Testing for H. pylori
There are several easy ways to get tested for an H. pylori infection by your healthcare provider.
Breath Test
This test is able to identify most people with H. pylori. To take the test, your healthcare provider will have you swallow a solution that contains urea. If H. pylori is present, the bacteria will convert the urea into carbon dioxide after about 10 minutes. Determining whether you have H. pylori is then detected by measuring the amount of carbon dioxide exhaled.
This test can also be used to measure whether the infection has been successfully treated. The breath test for H. pylori is most effective if you have been experiencing symptoms for about six months or less.
Blood Test
Blood tests are used to detect the presence of H. pylori antibodies. Antibodies are proteins made by the immune system made specifically to fight certain infections. Once your immune cells come into contact with bacteria, it creates specific antibodies for that bacteria so that it may fight it off more successfully.
After an extended period of time of being infected, the number of antibodies in the blood may begin to decline, which could result in the test having incorrect results.
Stool Testing
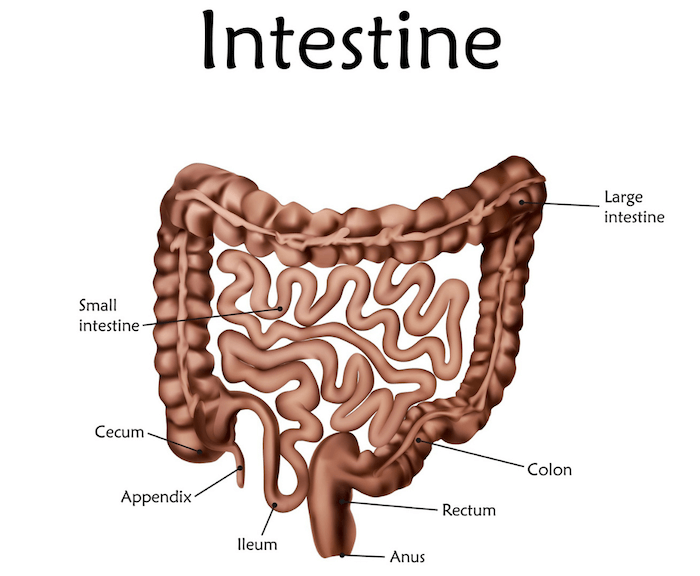
Stool tests can detect if there are traces of H. pylori in the feces. Since H. pylori resides in the stomach, the bacteria are able to travel through your digestive tract along with digested food. We all know where that ends up!
If treatment is successful, there will no longer be H. pylori present in the gut, so this method can also be used to confirm whether the infection is no longer active.
This testing method is best for chronic infection, where symptoms have been present for over six months.
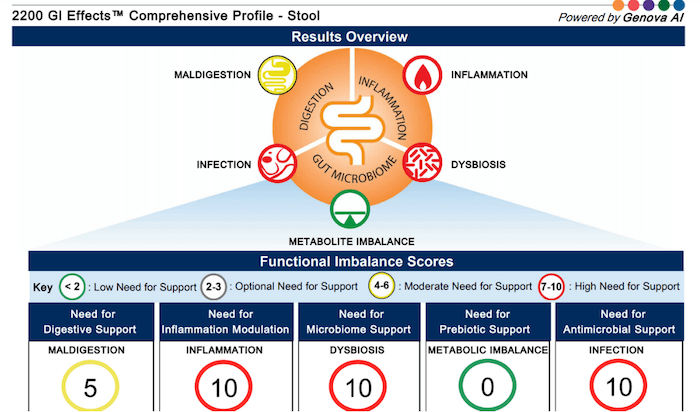
This is the testing method we use with clients because it also analyzes markers for maldigestion, inflammation, dysbiosis, metabolite imbalance, and other possible infections. We choose this method because it gives more information than just whether or not the H. pylori infection alone could be the root cause of your symptoms.
Endoscopic Exam
An endoscopic exam is a procedure where a small piece of tissue from the stomach lining is tested. This test is usually recommended by your healthcare provider in response to an ulcer, bleeding, or when checking for cancer. Since this examination is used to test for other issues within the gut, it can often miss the infection itself.
How is H. pylori transmitted?
The most common way to become infected with H. pylori is through consuming contaminated uncooked foods.
This infection can also be passed from person to person from direct contact with:
- Saliva (1/3 of all cases are caught through saliva/kissing)
- Oral cavity
- Vaginal and prostate fluids
- Fecal matter
Prevention of H. pylori

Since this is an infection primarily passed between food and people, H. pylori prevention has a lot to do with safe food preparation and cleanliness.
Some tips for preventing an H. pylori infection include:
- Wash your produce
- Wash your hands regularly, especially after using the restroom or handling uncooked foods
- Make sure all food is thoroughly cooked
- Avoid food and water that is not clean
With these easy practices, you can protect yourself from H. pylori and many other types of harmful bacteria!
Symptoms of H. pylori infection

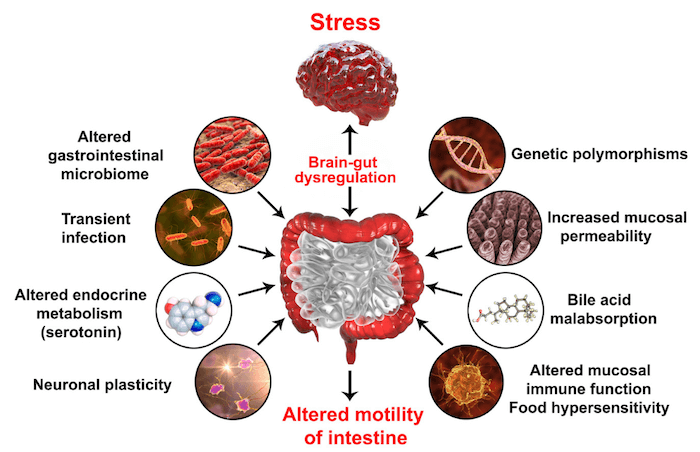
Since the inflammation response to H. pylori is ineffective, the body is left in a state where it is constantly inflamed. Chronic inflammation is stressful on the body because it knows that the bacteria is still there.
If left inflamed for too long, the body will begin to damage healthy cells within the digestive tract.
Digestion and malabsorption-related symptoms of H. pylori:
- Belching
- Nausea
- Constipation
- Upper abdominal pain
- Heartburn or acid reflux
- Gastritis
- Indigestion
- Amino acid deficiencies
- Depression
- Joint pain
- An ongoing need for HCl or digestive enzymes
- Weak immune system
- Fatigue
- Unstable blood sugar
Symptoms can occur in clusters as well as change over time.
Other consequences of H. pylori

A common failure for diagnosis is that H. pylori can manifest in symptoms that lie outside of the digestive tract such as bladder infections, insomnia, and anxiety.
These types of symptoms can make it difficult to pinpoint the infection as the root cause, so it is important to express when your symptoms first started as well as what was going on in your life at the time.
Extended inflammation can also lead to more serious problems because of the damage done to your cells.
Examples of less common, but more serious, effects of an H. pylori infection are:
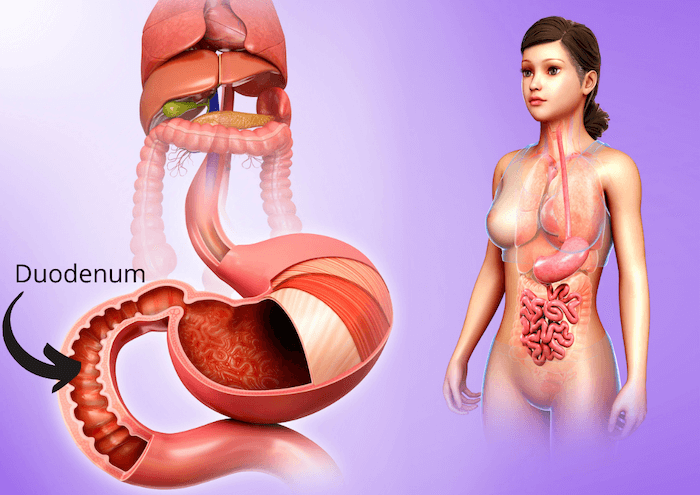
- Duodenal or peptic ulcers
- Mucosa-associated lymphoid tissue (MALT) lymphoma
- Gastric adenocarcinoma
H. pylori infections are the strongest risk factor for gastric cancer – nearly 75% of all gastric cancer cases can be attributed to H. pylori. This is why it is so important to seek help if you are feeling any symptoms of an H. pylori infection – you need to treat the inflammation before it becomes a more serious concern.
Co-occurring conditions are more likely if infected with H. pylori
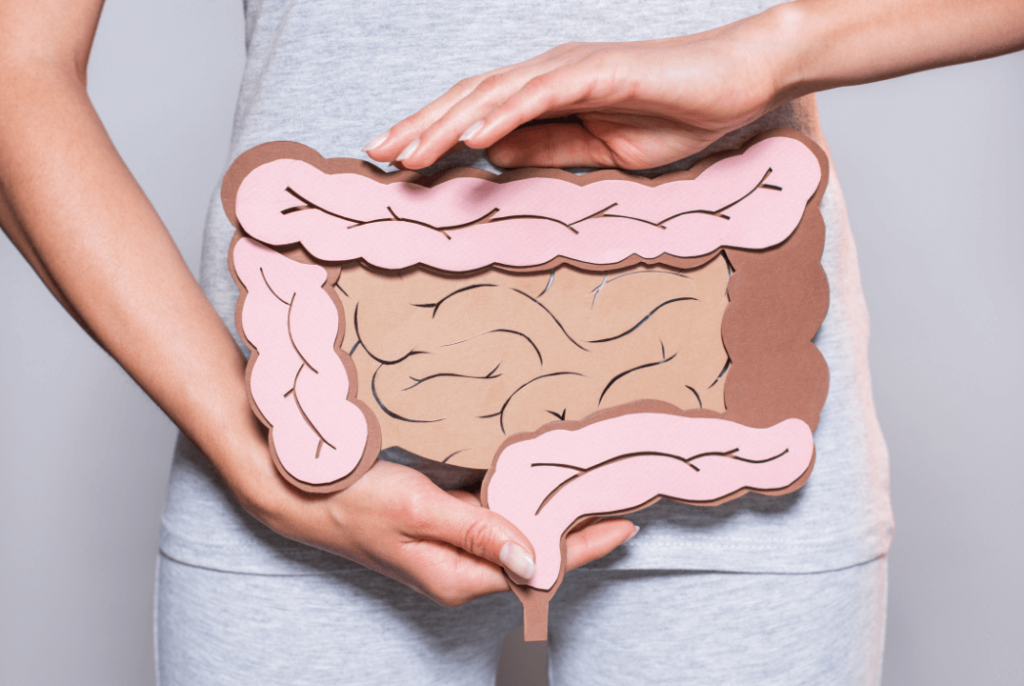
Another important thing to consider is that H. pylori may not be the only factor at play in your digestive struggles.
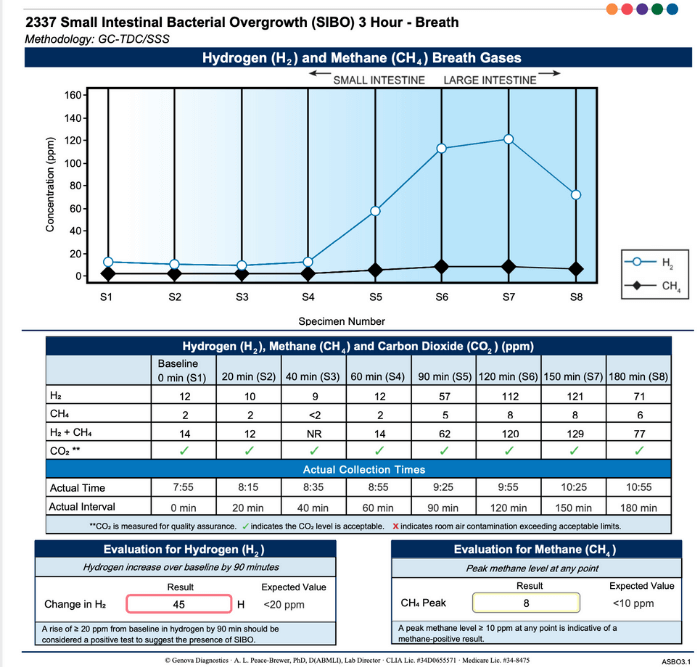
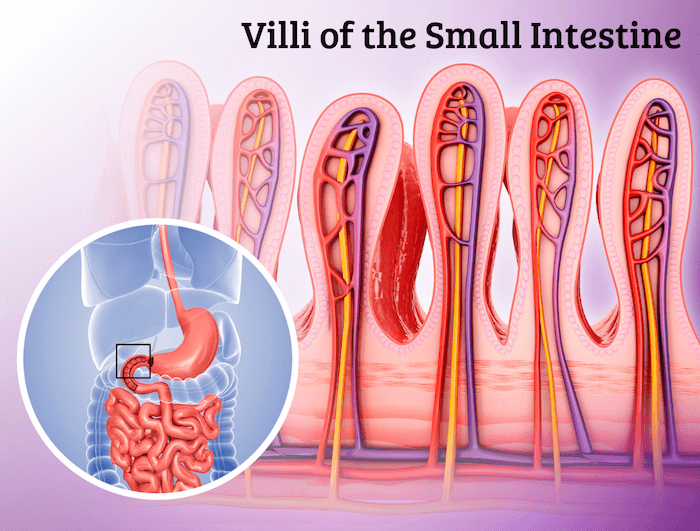
Since this infection lowers stomach acid, it also makes it easier for other infections and overgrowths to take place within the digestive tract. Many times, we will see both H. pylori and other conditions, such as small intestinal bacterial overgrowth (SIBO), co-occurring.
If your digestion is out of whack, you should consider getting tested for more than one kind of infection/overgrowth.
If you have both SIBO and H. pylori, H. pylori should be treated first because it occurs earlier in the digestive tract. H. pylori lives in the stomach, while SIBO takes place in the small intestine, and the acidity in the stomach is necessary to heal and prevent SIBO.
Treatment for H. pylori
The conventional method of healing H. pylori is through the use of antibiotics, but this does not always fully treat the infection or address the consequences of the infection. Doctors may prescribe Prevpac for about 2 weeks along with an anti-inflammatory diet.
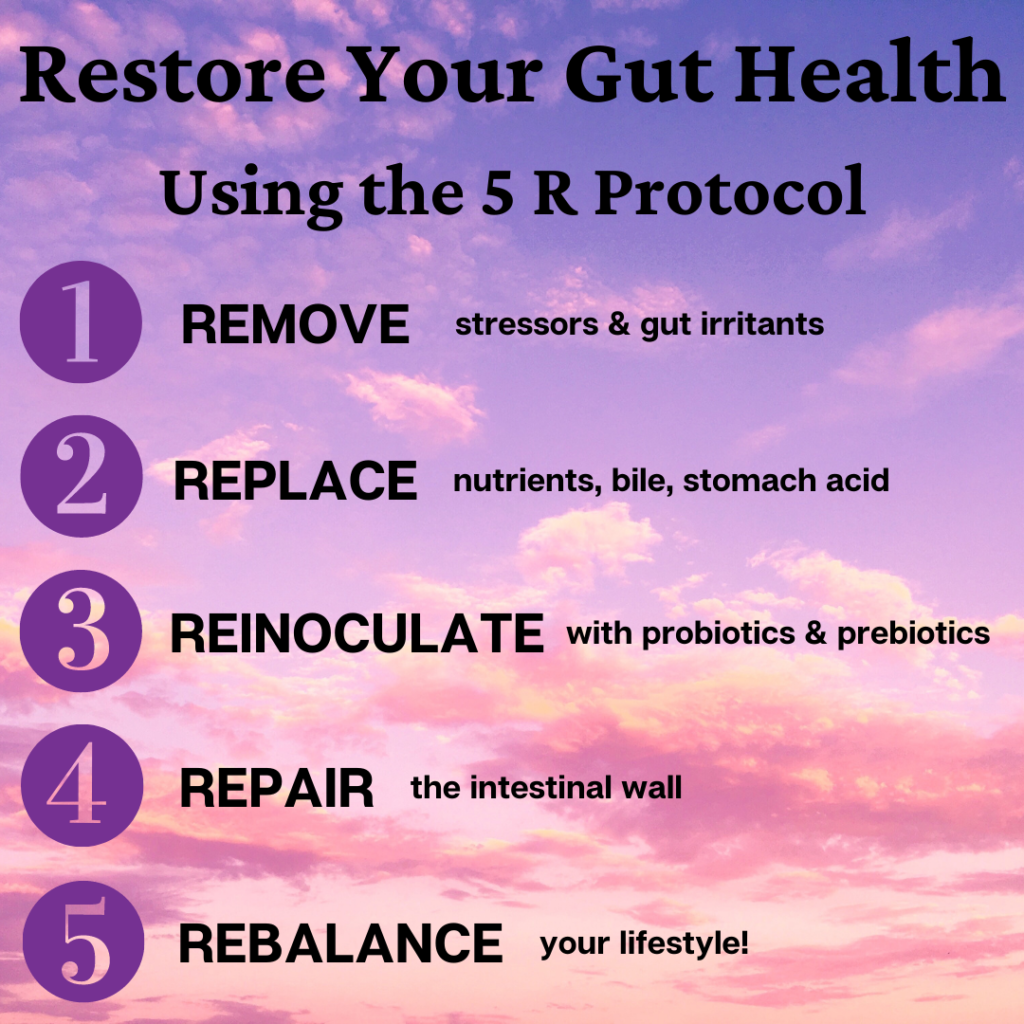
Our approach involves addressing the full spectrum, starting with why the infection was allowed to take place (the root cause) and ending with the symptoms and other consequences of infection.
The following protocol can be utilized to fully treat and heal your body.
Stage 1: Stress Management and Adrenal Support
The first step is to resolve any factors that may be causing any additional inflammation. This process focuses on individualized dietary and lifestyle changes. Our team will work with you to discover your personal needs in order to help you find the support program that will work best for you!
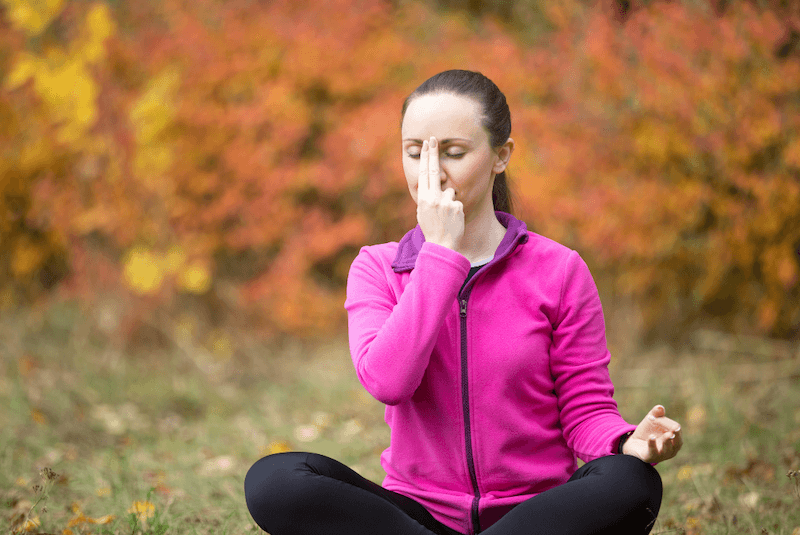
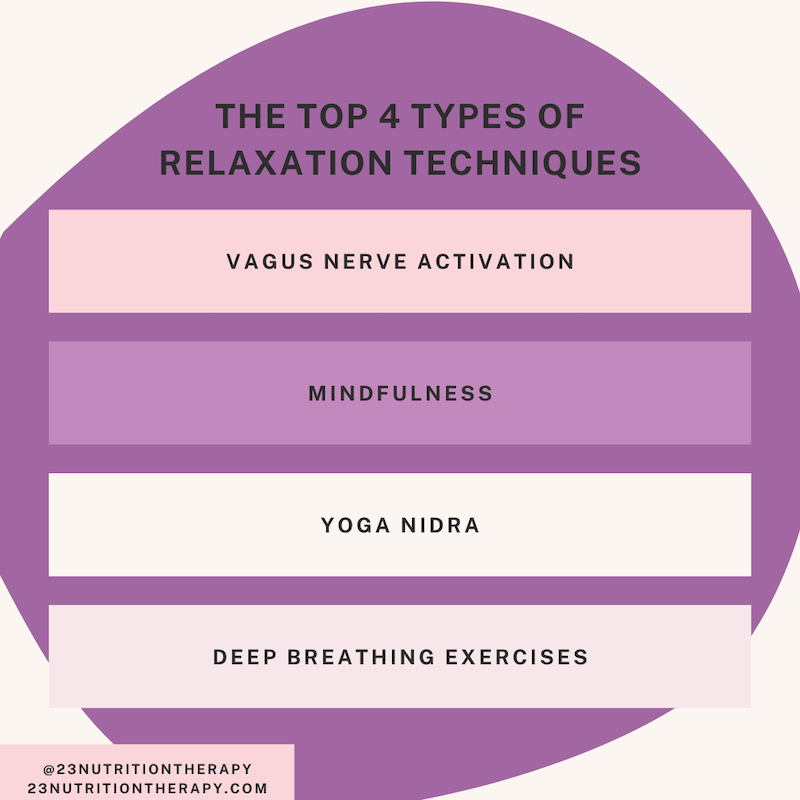
The Importance of Stress Reduction
Reducing stress supports the adrenals and helps to reduce both inflammation and symptoms of an H. pylori infection. Practicing mindfulness and incorporating new stress management techniques train the body to better recognize that it is not in danger, allowing the body to relax more easily.
Reducing inflammation is essential for treating an H. pylori infection, and strengthens the overall health of your gut. Stress negatively impacts every step of the digestive process, and can also lower stomach acid levels. This is why it is so important to address stress when healing H. pylori: the effects of each can compound on each other and make you feel even worse.
After incorporating stress-reducing and anti-inflammatory practices for about 60 days, you can move onto stage 2 of your treatment protocol. Following an anti-inflammatory diet can also be helpful in reducing any irritants to your gut, reducing the severity of painful symptoms.
Adrenal Support for Healing H. pylori
One common effect of H. pylori is adrenal dysfunction (aka adrenal fatigue). Your adrenal glands produce hormones that allow your body to work through stressful situations. After prolonged periods of stress, such as from having an H. pylori infection, you can experience adrenal burnout symptoms including fatigue, brain fog, or widespread inflammation.
Participating in our personalized Adrenal Reboot Program can help to reset your stress response system, reduce inflammation, and alleviate symptoms of burnout. Another option is our app-based Adrenal Cleanse protocol, more suitable for those who feel they need less personalized support. We also recommend testing for possible food allergies and sensitivities. It’s possible that consuming certain foods results in additional, unnecessary inflammation within your body.
Stage 2: Treatment phase – Eliminating H. pylori
After strengthening the digestive system through stress management, it is now time to move onto killing the H. pylori infection. Antibiotics can be used, but there is also a more natural approach. These two methods can also be used together if they are determined as the most effective form of treatment by your healthcare provider.
Herbal treatment of H. pylori may include:
- Mastica/mastic gum
- Slippery elm
- Deglycyrrhizinated Licorice Root Extract (DGL)
- Zinc carnosine
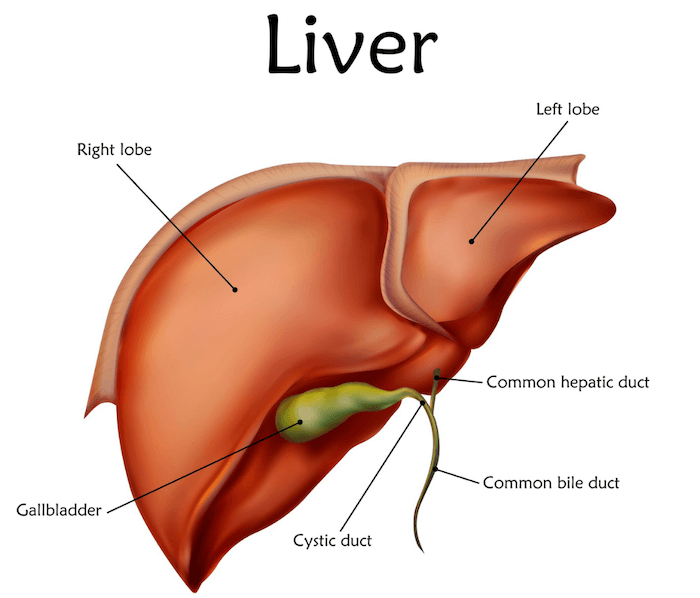
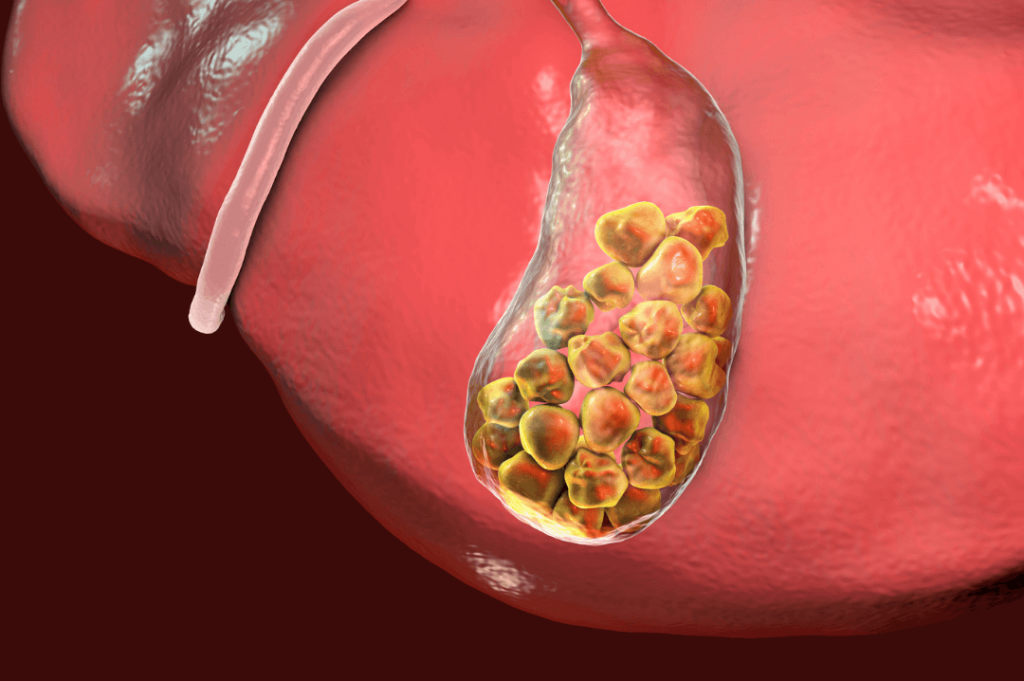
During this step, you may need to support your liver detox pathways because H. pylori can be transmitted to the liver through the blood. Extra support will aid in helping against any deterioration of liver function potentially caused by the infection.
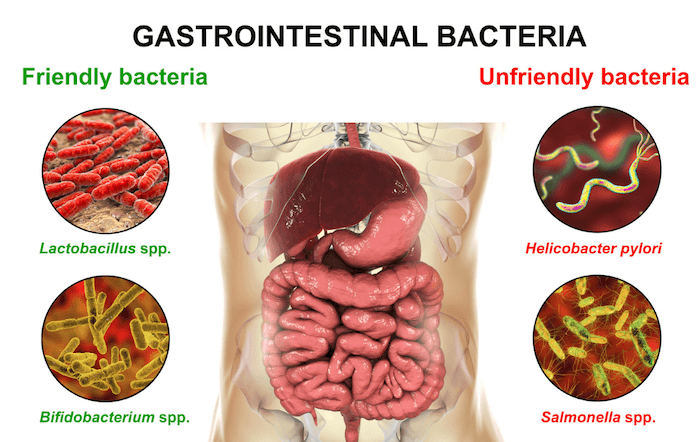
3. Replace healthy bacteria
After successfully killing off your H. pylori infection, it is now time to repair your gut and rebuild any deficits in order to protect from future infections by maximizing gut function. In this step, probiotics (usually multi-strain, high potency) are introduced.
Probiotics are called “good bacteria” because they help fight off bad bacteria and help keep your gut microbiome well-regulated. This is also a good time to begin taking a gastrointestinal (GI) repair powder, glutamine plus herbal support, to repair any damaged GI tissues.
After this step, we recommend retesting in order to verify that you are no longer carrying H. pylori and that probiotics, the healthy bacteria, have recolonized the GI tract. If your test results show that this is true, your GI tissue is on the road to recovery and the treatment has been successful in healing H. pylori.
If you happen to also be suffering from another pathogen in your GI tract, it is now possible to begin treatment to restore your gut health back to optimal function.
Working with a skilled practitioner is essential to ensure optimal results, as both the dosage and the length of the protocol matter for lasting success. The treatment process takes patience and ongoing support, and having someone to guide you can help keep you on track!
If you’ve been having digestive distress and think H. pylori may be the culprit – schedule a free 15-minute discovery call and we can discuss how to plan out the best approach for you!