The Gluten-Free Switch
What is MRT Testing and the LEAP Therapy Immunocalm Diet
Since you’re reading this, you may be dealing with uncomfortable post-meal symptoms and are trying to find out the cause. This article will walk you through our favorite method to test for food sensitivities: MRT food sensitivity testing.
With so many foods and chemicals available today, chances are you have experienced unpleasant symptoms after a meal but can’t pinpoint the exact cause. While these symptoms are not typically life-threatening, they can disrupt your life with uncomfortable symptoms. This is because the body’s immune reaction generates feelings of fatigue, bloating, gas, stomach pain, brain fog, and more.
While one common recommendation for food sensitivities is doing an elimination diet and keeping a food journal; this approach can often be tedious and not reliable. Think about it… If your food sensitivity is due to a chemical used in a particular food, there is no way you can detect that specific chemical from an elimination diet alone. This is why I want to introduce to you the Mediator Release Test (MRT). This article will explain to you why this combo of MRT coupled with the LEAP protocol (Lifestyle Eating And Performance) is highly effective at detecting personalized food sensitivities.
Inflammation and Food Sensitivities
 In the broad sense, food sensitivity refers to the body’s adverse reaction to specific food or chemical antigens (also known as a toxin or foreign substances) causing negative physiological effects within the body. The term “food sensitivity” specifically refers to a delayed, dose-dependent, adverse reaction to food.
In the broad sense, food sensitivity refers to the body’s adverse reaction to specific food or chemical antigens (also known as a toxin or foreign substances) causing negative physiological effects within the body. The term “food sensitivity” specifically refers to a delayed, dose-dependent, adverse reaction to food.
In simpler terms, your uncomfortable symptoms occur a while after consumption and also depend on how much you eat. This physiological reaction involves the immune system’s white blood cells (WBCs) and functions in the production of inflammatory mediators that ultimately cause the symptoms of food sensitivities.
Release of Mediators Lead to Food Sensitivities and Inflammation
In short, when we eat foods or chemicals that our bodies are sensitive to, our WBCs will be triggered to release various mediators such as histamine, cytokines, prostaglandins, leukotrienes, and up to 97 others into the bloodstream. As a result, the mediators that are released into the bloodstream usually cause subtle, unpleasant, or disruptive symptoms throughout the body.
To put this concept into perspective, a common food sensitivity is gluten. Gluten sensitivity often causes abdominal pain, bloating, diarrhea, and brain fog after consuming moderate amounts. What’s most important to recognize from this example is that the mediators that are released are not localized to a single organ. But rather, they circulate throughout the body causing a multitude of symptoms.
With that said, you may have experienced a similar situation, which can be very frustrating when trying to figure out exactly what is causing your symptoms. Luckily, a test known as the mediator release test (MRT) can be very helpful with determining not only if your symptoms are food-related, but also identifying specifically which foods or chemicals are the root cause.
Why Test MRT?
Now that we know what mediators are, how they are released, and what functions they have on our body, it makes sense that the most accurate food sensitivity test would focus on mediators. The test that we use to test food sensitivities is called the mediator release test (MRT). This test involves drawing blood (at a facility or with a mobile phlebotomist) and then having that blood sample shipped overnight to a lab. Once in the lab, it will be divided and mixed with high-quality freeze-dried food/chemical antigens that are tested on the MRT panel.
The next step of the MRT food sensitivity test is to analyze the mixed-blood samples by using the technology of flow cytometry and impedance technology to measure the liquid-to-solid ratio. What this means is that when a WBC reacts to a certain food antigen found within the mixture, there will be an increased amount of mediators released from the WBC which ultimately causes the WBC to shrink in size. While this food antigen response is a normal physiological process that constantly happens within the body, when a food sensitivity is detected, the WBC mediator’s response actually reacts in the form of a threat and is elevated to much higher levels than normal.
How Does MRT Food Sensitivity Testing Work?
The good news is these mediator response levels are exactly what MRT food sensitivity testing assesses. The test will quantify the level of food and chemical reactivity in the form of a standard deviation bell curve for your functional medicine practitioner or certified LEAP therapist to better analyze. The goal is to choose the lowest inflammatory foods while providing a balanced diet with a variety of foods. How it works is the standard deviation graph values represent a bell curve ranging from 0.0 to 2.0. Within those values, any food item with a reactive value of 0.0 will have a negligible bar graph, 0.5 is ¼ of the way up the “green” bar graph, 1.0 is halfway across, 1.5 is ¾ of the way across, and 2.0 is the highest level of the bar graph.
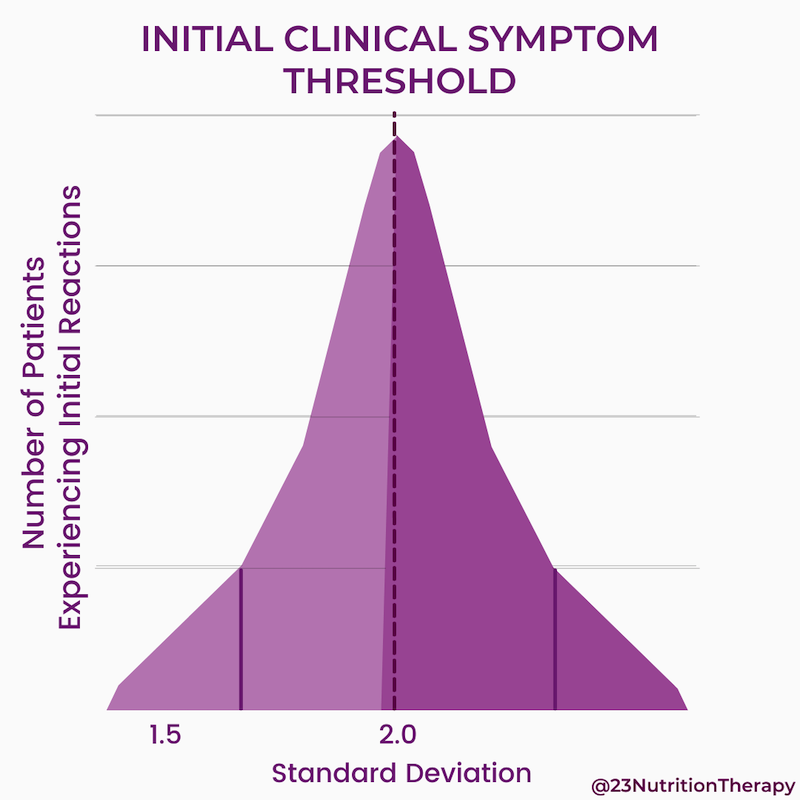
While manifestations of symptoms are most commonly seen after the 2.0 threshold, individual variations occur. For example, some people may have symptoms from foods slightly below 2.0. Others might not notice symptoms until the reactions are in the “yellow” range. In other words, food choices should ideally consist of items that have a reactive value of 1.0 or below. However everyone’s body is unique, and as mentioned before, food sensitivities are both dose- and frequency-dependent.
Therefore, with the help of your functional medicine dietitian and certified LEAP therapist, you will better understand your personal threshold with the results from the standard deviation graph and use it in your lifestyle, eating, and performance (LEAP) protocol. With the LEAP protocol, you will work to formulate a customized diet plan to meet your individual needs while avoiding foods or chemicals that are triggering.
MRT Food Sensitivity Testing Reliability
Why did I say the MRT blood test is the most accurate? Well, compared to other food sensitivity tests that are outdated or focus on only one sensitivity metric like IgG antibodies, the MRT is highly reliable due to its capacity to measure the exact cause of food sensitivities in the form of all mediators and antibodies released.
In addition, the MRT blood test is very accurate with a sensitivity rating reaching 95% and a specificity of 92%. (1) Likewise, MRT has proven to have a reproducibility constant of 90% of the time. In other words, out of every 10 people being tested, 9 of them will consistently obtain the same lab results. This helps eliminate false-positive discrepancies.
Why do I Have So Many Food Sensitivities?
One thing to know about adverse food reactions is about 50 to 90% are actually due to sensitivities or intolerances. (1) In fact, one major cause of food sensitivities is actually occurring because of poor gut barrier function aka “leaky gut”. Leaky gut occurs due to irritants such as food antigens (gluten for example) causing an inflammatory response on the gastrointestinal lining leading to mucosal tissue damage.
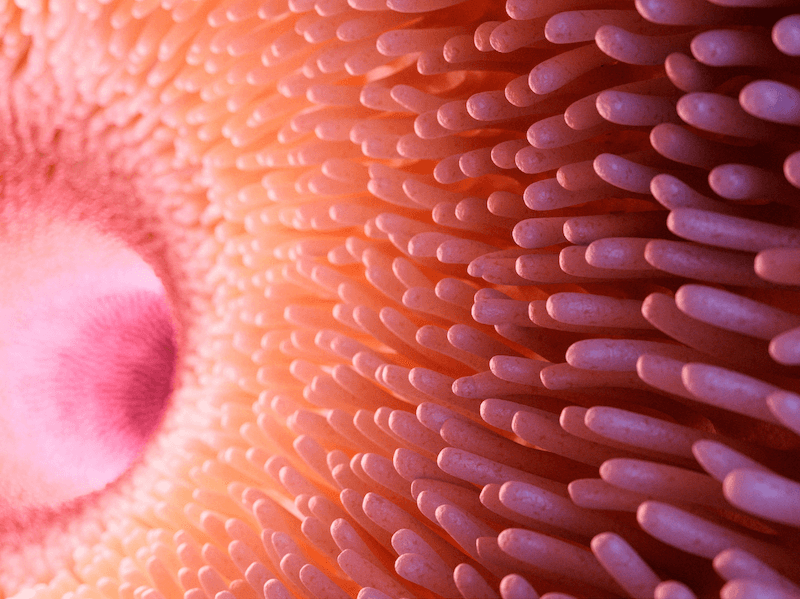
What this means is through the inflammatory response these food antigens destroy our intestinal villus which is the absorption site of our nutrients. It also means this inflammatory response is downregulating the gut’s first physical barrier of defense against pathogens, parasites, bacteria, and yeast known as the secretory immunoglobulin A (SIgA). Lastly, it means the inflammatory response is causing an erosion of the gut barrier’s tight junctions allowing for large undigested molecules in our bloodstream. (2) If you find you have many food sensitivities, the best place to start is healing the gut lining with a gut cleans diet by working with a functional medicine dietitian who is LEAP certified.
Why do Food Sensitivities Matter?
Without our villi properly absorbing nutrients and without SIgA protecting us from these pathogens, the gut’s permeability through tight junctions allows for undigested food and other toxins into our bloodstream which further perpetuates the inflammatory response. Remember what happens when we have an inflammatory response? White blood cells come to the scene and ultimately release our not-so-friendly friends, the mediators.
As mentioned before, the mediator response is not localized to a single organ and ultimately leads to uncomfortable symptoms and various disease states. Likewise, because the villi are not properly absorbing our nutrients we can also become malnourished, contributing to additional signs and symptoms.
The good news is this can be prevented with an MRT by identifying any food sensitivities and eliminating them through the diet. Next, you can begin repairing the leaky gut with the help of a functional medicine practitioner or certified LEAP therapist by incorporating any supplementation into your LEAP protocol if necessary.
So, if you believe food may be contributing to your symptoms and you are having trouble pinpointing the root cause, a food sensitivity test might be beneficial for you. If you are wondering how some of these food sensitivities manifest, the following symptoms and conditions are a good indicator you may be dealing with food sensitivity and MRT food sensitivity testing might be right for you.
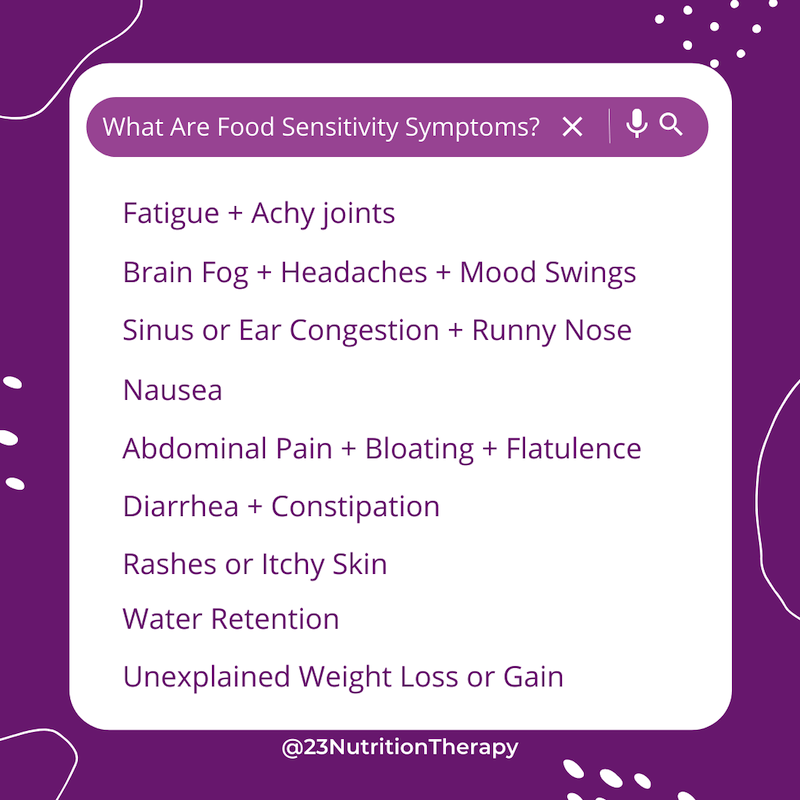
Food sensitivity symptoms can include:
- Fatigue, achy joints
- Brain fog, headaches, mood swings
- Sinus or ear congestion, runny nose
- Nausea, unexplained weight loss or gain
- Abdominal pain, bloating, flatulence
- Diarrhea, constipation
- Rashes or itchy skin
- Water retention
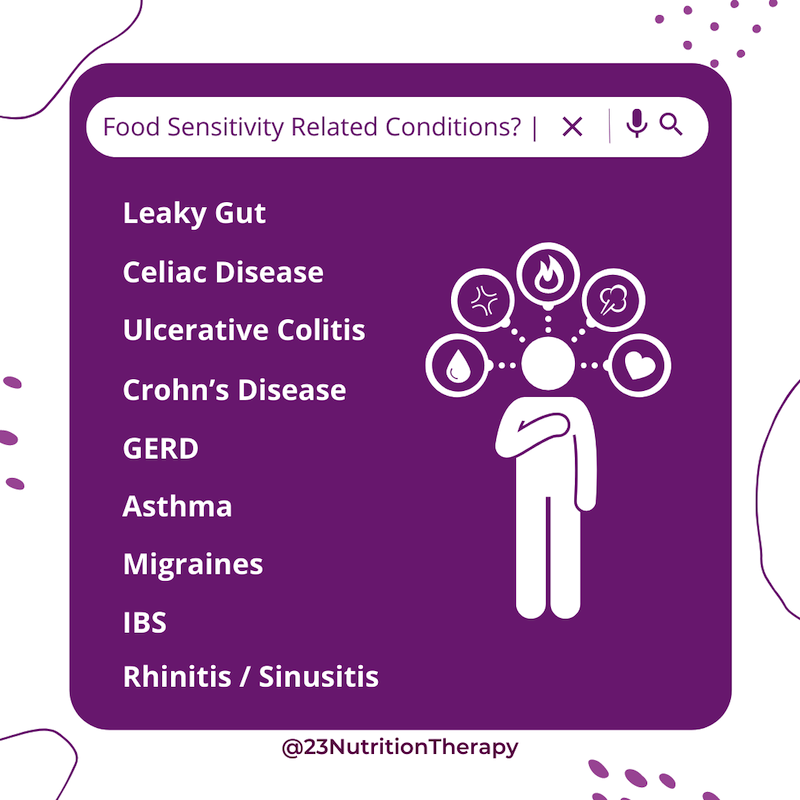
Food sensitivity-related conditions can include:
- Celiac disease
- Ulcerative colitis
- Crohn’s disease
- GERD
- Asthma
- Migraines
- Leaky Gut
- IBS
- Rhinitis/Sinusitis
What is the LEAP Diet Protocol?
LEAP stands for lifestyle, eating, and performance diet protocol. The LEAP protocol as briefly talked about is based on the information provided by your MRT food sensitivity testing results, and is used as the new foundation to health and recovery. Unlike a typical elimination diet and food journal; the LEAP protocol entails a multiphase approach (usually 3 phases total) with an initial immuno-calm phase to drastically reduce inflammation. This is then followed by the incorporation of safe foods while temporarily eliminating sensitive foods.
Therefore, with the help of a functional medicine dietitian who is certified as a LEAP therapist, the LEAP protocol is used to selectively expand on acceptable food options to ultimately develop a flexible and nutrient-dense food plan that is free from adverse food reactions. Depending on your case, you may also be given lifestyle strategies to minimize symptoms, repair your digestion, and restore your gut health.
What’s Next?
If you’re tired of not feeling your ultimate best, and feel like any of the symptoms or conditions I provided relate to you, then it’s time to let the science talk. With MRT food sensitivity testing, not only will you obtain personalized results, but with the help of a functional medicine dietitian and certified LEAP therapist, you can begin enjoying food again without the fear of adverse food reactions.
LEAP Immunocalm diet package and mediator release test cost?
Take the LEAP symptom assessment to determine if LEAP is something that could work for you! If you find that you are scoring high, you may need to Schedule your appointment today to speak with a LEAP dietitian and begin your journey to wellness!
Resources
Healing H. pylori with Nutrition Therapy
Have you been suffering from sharp pains or burning in your abdomen that just won’t go away? Is this pain making it difficult to complete your daily activities? You may have caught an H. Pylori infection. Healing H. pylori requires guidance from a skilled healthcare practitioner. So don’t worry, we will have you feeling better in no time!
What is Helicobacter pylori?
Helicobacter pylori is a type of bacteria that lives within the stomach. It releases toxins into the lining of the stomach, going through several layers of mucus and stomach tissue. This causes damage to the stomach lining and reduces stomach acid production.
Stomach acid is necessary to break down proteins, and low stomach acid means food is not digested as fully or efficiently as it would under normal conditions. This affects amino acid absorption, meaning the body is not able to absorb all the nutrients from your food, impacting every cell in the body.
By limiting amino acid absorption, an H. pylori infection can impact the production of:
- Antibodies/Immunoglobulins (responsible for fighting against infection)
- All enzymes (responsible for energy production and other bodily processes)
- Thyroid hormones, insulin, follicle-stimulating hormone, and all other amino acid-based hormones
- Hemoglobin and ferritin (store critical proteins transported to all cells and tissues)
- Neurotransmitters
The body tries to fight against these toxins by using inflammation as a natural defense. Inflammation is a common response to any type of trauma to the body because it wakes up the immune system and encourages phagocytes, your own personal fighter cells, to come to the area.
The resulting inflammation may be responsible for the pain that you may be feeling from the infection. Unfortunately, the H. pylori bacterium has evolved to be prepared for the inflammation response and is immune to it, allowing for the infection to persist if not treated properly.
Testing for H. pylori
There are several easy ways to get tested for an H. pylori infection by your healthcare provider.
Breath Test
This test is able to identify most people with H. pylori. To take the test, your healthcare provider will have you swallow a solution that contains urea. If H. pylori is present, the bacteria will convert the urea into carbon dioxide after about 10 minutes. Determining whether you have H. pylori is then detected by measuring the amount of carbon dioxide exhaled.
This test can also be used to measure whether the infection has been successfully treated. The breath test for H. pylori is most effective if you have been experiencing symptoms for about six months or less.
Blood Test
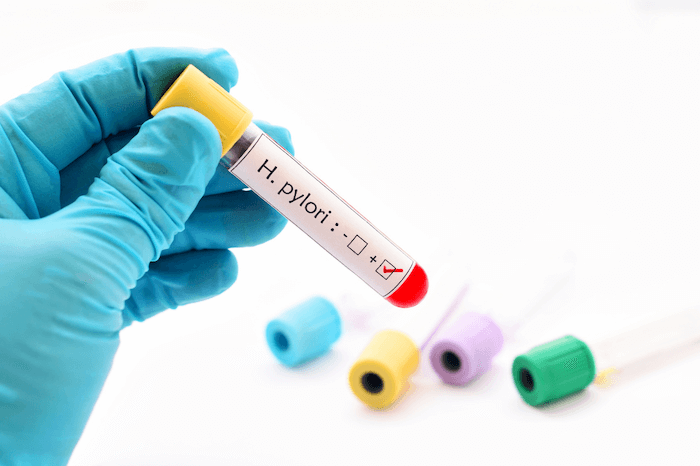
Blood tests are used to detect the presence of H. pylori antibodies. Antibodies are proteins made by the immune system made specifically to fight certain infections. Once your immune cells come into contact with bacteria, it creates specific antibodies for that bacteria so that it may fight it off more successfully.
After an extended period of time of being infected, the number of antibodies in the blood may begin to decline, which could result in the test having incorrect results.
Stool Testing
Stool tests can detect if there are traces of H. pylori in the feces. Since H. pylori resides in the stomach, the bacteria are able to travel through your digestive tract along with digested food. We all know where that ends up!
If treatment is successful, there will no longer be H. pylori present in the gut, so this method can also be used to confirm whether the infection is no longer active.
This testing method is best for chronic infection, where symptoms have been present for over six months.
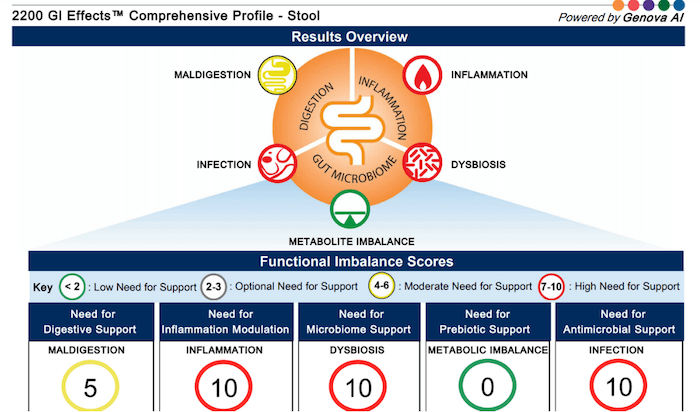
This is the testing method we use with clients because it also analyzes markers for maldigestion, inflammation, dysbiosis, metabolite imbalance, and other possible infections. We choose this method because it gives more information than just whether or not the H. pylori infection alone could be the root cause of your symptoms.
Endoscopic Exam
An endoscopic exam is a procedure where a small piece of tissue from the stomach lining is tested. This test is usually recommended by your healthcare provider in response to an ulcer, bleeding, or when checking for cancer. Since this examination is used to test for other issues within the gut, it can often miss the infection itself.
How is H. pylori transmitted?
The most common way to become infected with H. pylori is through consuming contaminated uncooked foods.
This infection can also be passed from person to person from direct contact with:
- Saliva (1/3 of all cases are caught through saliva/kissing)
- Oral cavity
- Vaginal and prostate fluids
- Fecal matter
Prevention of H. pylori

Since this is an infection primarily passed between food and people, H. pylori prevention has a lot to do with safe food preparation and cleanliness.
Some tips for preventing an H. pylori infection include:
- Wash your produce
- Wash your hands regularly, especially after using the restroom or handling uncooked foods
- Make sure all food is thoroughly cooked
- Avoid food and water that is not clean
With these easy practices, you can protect yourself from H. pylori and many other types of harmful bacteria!
Symptoms of H. pylori infection

Since the inflammation response to H. pylori is ineffective, the body is left in a state where it is constantly inflamed. Chronic inflammation is stressful on the body because it knows that the bacteria is still there.
If left inflamed for too long, the body will begin to damage healthy cells within the digestive tract.
Digestion and malabsorption-related symptoms of H. pylori:
- Belching
- Nausea
- Constipation
- Upper abdominal pain
- Heartburn or acid reflux
- Gastritis
- Indigestion
- Amino acid deficiencies
- Depression
- Joint pain
- An ongoing need for HCl or digestive enzymes
- Weak immune system
- Fatigue
- Unstable blood sugar
Symptoms can occur in clusters as well as change over time.
Other consequences of H. pylori

A common failure for diagnosis is that H. pylori can manifest in symptoms that lie outside of the digestive tract such as bladder infections, insomnia, and anxiety.
These types of symptoms can make it difficult to pinpoint the infection as the root cause, so it is important to express when your symptoms first started as well as what was going on in your life at the time.
Extended inflammation can also lead to more serious problems because of the damage done to your cells.
Examples of less common, but more serious, effects of an H. pylori infection are:
- Duodenal or peptic ulcers
- Mucosa-associated lymphoid tissue (MALT) lymphoma
- Gastric adenocarcinoma
H. pylori infections are the strongest risk factor for gastric cancer – nearly 75% of all gastric cancer cases can be attributed to H. pylori. This is why it is so important to seek help if you are feeling any symptoms of an H. pylori infection – you need to treat the inflammation before it becomes a more serious concern.
Co-occurring conditions are more likely if infected with H. pylori
Another important thing to consider is that H. pylori may not be the only factor at play in your digestive struggles.
Since this infection lowers stomach acid, it also makes it easier for other infections and overgrowths to take place within the digestive tract. Many times, we will see both H. pylori and other conditions, such as small intestinal bacterial overgrowth (SIBO), co-occurring.
If your digestion is out of whack, you should consider getting tested for more than one kind of infection/overgrowth.
If you have both SIBO and H. pylori, H. pylori should be treated first because it occurs earlier in the digestive tract. H. pylori lives in the stomach, while SIBO takes place in the small intestine, and the acidity in the stomach is necessary to heal and prevent SIBO.
Treatment for H. pylori
The conventional method of healing H. pylori is through the use of antibiotics, but this does not always fully treat the infection or address the consequences of the infection. Doctors may prescribe Prevpac for about 2 weeks along with an anti-inflammatory diet.
Our approach involves addressing the full spectrum, starting with why the infection was allowed to take place (the root cause) and ending with the symptoms and other consequences of infection.
The following protocol can be utilized to fully treat and heal your body.
Stage 1: Stress Management and Adrenal Support
The first step is to resolve any factors that may be causing any additional inflammation. This process focuses on individualized dietary and lifestyle changes. Our team will work with you to discover your personal needs in order to help you find the support program that will work best for you!
The Importance of Stress Reduction
Reducing stress supports the adrenals and helps to reduce both inflammation and symptoms of an H. pylori infection. Practicing mindfulness and incorporating new stress management techniques train the body to better recognize that it is not in danger, allowing the body to relax more easily.
Reducing inflammation is essential for treating an H. pylori infection, and strengthens the overall health of your gut. Stress negatively impacts every step of the digestive process, and can also lower stomach acid levels. This is why it is so important to address stress when healing H. pylori: the effects of each can compound on each other and make you feel even worse.
After incorporating stress-reducing and anti-inflammatory practices for about 60 days, you can move onto stage 2 of your treatment protocol. Following an anti-inflammatory diet can also be helpful in reducing any irritants to your gut, reducing the severity of painful symptoms.
Adrenal Support for Healing H. pylori
One common effect of H. pylori is adrenal dysfunction (aka adrenal fatigue). Your adrenal glands produce hormones that allow your body to work through stressful situations. After prolonged periods of stress, such as from having an H. pylori infection, you can experience adrenal burnout symptoms including fatigue, brain fog, or widespread inflammation.
Participating in our personalized Adrenal Reboot Program can help to reset your stress response system, reduce inflammation, and alleviate symptoms of burnout. Another option is our app-based Adrenal Cleanse protocol, more suitable for those who feel they need less personalized support. We also recommend testing for possible food allergies and sensitivities. It’s possible that consuming certain foods results in additional, unnecessary inflammation within your body.
Stage 2: Treatment phase – Eliminating H. pylori
After strengthening the digestive system through stress management, it is now time to move onto killing the H. pylori infection. Antibiotics can be used, but there is also a more natural approach. These two methods can also be used together if they are determined as the most effective form of treatment by your healthcare provider.
Herbal treatment of H. pylori may include:
- Mastica/mastic gum
- Slippery elm
- Deglycyrrhizinated Licorice Root Extract (DGL)
- Zinc carnosine
During this step, you may need to support your liver detox pathways because H. pylori can be transmitted to the liver through the blood. Extra support will aid in helping against any deterioration of liver function potentially caused by the infection.
3. Replace healthy bacteria
After successfully killing off your H. pylori infection, it is now time to repair your gut and rebuild any deficits in order to protect from future infections by maximizing gut function. In this step, probiotics (usually multi-strain, high potency) are introduced.
Probiotics are called “good bacteria” because they help fight off bad bacteria and help keep your gut microbiome well-regulated. This is also a good time to begin taking a gastrointestinal (GI) repair powder, glutamine plus herbal support, to repair any damaged GI tissues.
After this step, we recommend retesting in order to verify that you are no longer carrying H. pylori and that probiotics, the healthy bacteria, have recolonized the GI tract. If your test results show that this is true, your GI tissue is on the road to recovery and the treatment has been successful in healing H. pylori.
If you happen to also be suffering from another pathogen in your GI tract, it is now possible to begin treatment to restore your gut health back to optimal function.
Working with a skilled practitioner is essential to ensure optimal results, as both the dosage and the length of the protocol matter for lasting success. The treatment process takes patience and ongoing support, and having someone to guide you can help keep you on track!
If you’ve been having digestive distress and think H. pylori may be the culprit – schedule a free 15-minute discovery call and we can discuss how to plan out the best approach for you!
Substitute Chinese Forbidden Rice for a More Exotic Dish!
The Bran layer between the rice grain and the outer hull gives black rice its nutritional kick. Black rice bran inhibits histamine and can reduce inflammation due to the high antioxidant content.
Studies in animals also indicate that black rice can lower atherosclerotic plaque, raise HDL cholesterol levels and lower LDL cholesterol levels, due to the high fiber. Forbidden black rice has both water-soluble and fat-soluble antioxidants, including vitamin E and anthocyanins, which have been linked to decreased risk of heart disease and cancer.
Try this recipe for Indonesian Black Sticky Rice Pudding! It’s so tasty!!!
- 1 1⁄4 cup of black glutinous/sticky rice • 11⁄4 cup of water
- 4 tbsp. palm sugar, divided
- 1 13.5oz can coconut milk
- Pinch of salt
- 1 vanilla bean
- 1 1⁄2 tsp. cornstarch
- 1⁄2 cup of dried unsweetened shredded coconut
- Soak rice in a large bowl and cover for 4-6 hours, then rice under cold water
- Add rice to sauce pan and bring to a boil, add 1 tbsp. of sugar, reduce heat and simmer until water is absorbed, remove from heat covered and rest for 10 min
- Bring coconut milk to a boil, add remaining sugar and salt, and reducing to a boil, then cut the vanilla bean, scrape out the seeds then add the seeds and pod to the mixture
- Make a dispersion of cornstarch with 1 tbsp. of cold water, then add to coconut mixture, stir on heat until thickened
- Toast shredded coconut separately
- Plate
- Serve!!!
Lowering Blood Pressure with Beetroot Juice

Most people know that it is important to include vegetables in our diet due to the health benefits of high fiber, vitamins, minerals, and antioxidants.
But did you know that many vegetables, particularly red beetroots and leafy greens, are very high in dietary nitrates? What is so important about dietary nitrates?
These dietary nitrates play a cardio-protective role by lowering blood pressure, reducing the inflammation response, and improving endothelial function. The body metabolizes dietary nitrates (NO3-) by first converting it to the biologically active form (NO 2 ), and then to Nitric oxide (NO).
Nitric oxide is a vasodilator and is responsible for regulating blood flow, muscle contractions, glucose and calcium homeostasis, as well as cellular respiration in the mitochondria. Previously it was though that dietary nitrates could not influence nitric oxide production, however new research challenges that and suggests that beetroot juice has a direct relationship on lowering systolic blood pressure.
Beets are also rich in betaine, which gives it that vibrant red color and has been used in cardiovascular treatments. These high antioxidants also aid in protecting against oxidative stress in the body.
Dietary nitrate supplementation has been shown to increase athletic performance by improving oxygen efficiency, reducing the amount of Oxygen needed to perform the same amount of work. Low levels of nitric oxide has been associated with hypertension and even elevated cholesterol.
Some factors that can alter the nitrate content in vegetables include environmental factors such as humidity, amount of sunlight, and water, pesticides and the genetics of the plant.
Consumers should be cautious however, about proper storage of high nitrate containing vegetable juices. Improper storage can accumulate large amounts of bacteria that accumulate nitrite buildup, which can become harmful. High amounts of nitrite have toxic and even deadly effects, which are seen in nitrate and nitrite containing drug use, such as nitroglycerine, and amyl nitrite.
Nitrites can also form N-nitrosamines in the body, which has been found to be carcinogenic in animals, but still has yet to proven in humans. While it is still unclear what the optimal level of daily dietary nitrate consumption is, the Dietary Approaches to Stop Hypertension (DASH) diet yields 20mmol of nitrate per day.
Current research studies are showing effective improvement of athletic ability, and decreased blood pressure with just 9 mmol (0.5 L beetroot juice or 300-500mg) nitrates daily.
Including vegetables in your diet that are highest in nitrates (>250mg/100g fresh weight) such as celery, cress, chervil, lettuce, red beetroot, spinach, and arugula can improve your overall cardiovascular health. This amount can easily be achieved with 1 cup of raw spinach containing 900mg nitrate, and a half a cup of cooked collard greens containing 200mg.
Recommendations on the amount of vegetables that are optimal for your health can be found in the Dietary Guidelines for Americans and the USDA’s MyPlate website.
References:
1. Coleman, E, MA, MPH, RD, CSSD. Beetroot Juice and Dietary Nitrates. The Integrative RDN. Spring
2016;18(4)98-104
2. USDA Choose Myplate website. http://www.choosemyplate.gov/. Published 2016. Accessed August 7,
2016