Do you ever feel sluggish, like your mood is all over the place, or generally notice you’re out of whack? A lot of our everyday functioning traces back to how well our brain is working. Neuronutrition is the concept of nourishing ourselves with the nutrients that are going to support our brain health.
That blob of gray matter between your ears, the brain, is actually the control center for your neurotransmitters. It controls the production of hormones, neurotransmitter communication, metabolism, and many other functions. What helps run these processes? Well, the foods we eat! Food can have a direct impact on the function of our brain.
It is important that we eat foods that provide us with the proper precursors (inactive substances converted to active ones such as an enzyme, vitamin, or hormone) for the neurotransmitters we require. Proper brain functioning helps us to regulate our three-body systems, as well as functions such as mood, sleep, and metabolism. But what does all this mean and how do you eat for your brain health? Let’s find out.
What Are Neurotransmitters?
There’s a good chance you’ve heard of neurotransmitters before, even if you have never actually seen this word! Neurotransmitters are brain chemicals created in our body that carry signals across brain cells or neurons. A few commonly discussed neurotransmitters include serotonin, dopamine, and norepinephrine.
Achieving and maintaining the optimal balance of these brain chemicals is essential for our mental health and mood. Food is one of the most direct ways that we can help balance our levels of neurotransmitters; in turn, helping us to regulate our mood, stress, anxiety, and even sleep.
Key Neurotransmitters and Their Function
Before diving into the important topic of neuro-nutrition, let’s set the stage with some important neurotransmitters you have probably heard of, and their main functions.
- Serotonin – Aids in regulating sleep/wake cycles and anxiety, mood behavior, appetite, and bowel contractions.
- Dopamine – Linked to focus, motivation, and pleasure.
- GABA – Helps regulate anxiety, stress levels, sleep/wake cycles, and calmness.
- Norepinephrine – Aids in attentiveness and focus.
Maintaining and restoring the balance between these neurotransmitters is oftentimes more important than focusing on stimulating a single pathway to produce or inhibit one neurotransmitter because these pathways are so interconnected. Here are a few examples of what different levels of these neurotransmitters can mean for our health: Low levels of serotonin have been linked to depression, anxiety and sleep issues. Excess dopamine can cause cells to experience cell death, or apoptosis, too early. Norepinephrine is commonly referred to as the “fight-or-flight” hormone (often called adrenaline), because it stimulates the sympathetic nervous system and makes us alert to potential danger. As you can see, it is crucial to keep our neurotransmitters in balance for various facets of our health.
 Foods For Neurotransmitters
Foods For Neurotransmitters
The neurotransmitters we need are made from the same building blocks as the rest of our cells. Think proteins, fats, vitamins, and minerals. We get these building blocks from our food! Therefore, certain nutrient-rich foods give us an advantage when it comes to building neurotransmitters. This is especially true because our gut actually has an important link to our neurotransmitters and brain health.
Phenylalanine is an amino acid that is the precursor, aka starting block, to proteins in our body and many of the neurotransmitters we’ve been discussing. We are unable to produce enough phenylalanine on our own, which makes it an essential amino acid that must be obtained through our diet. An essential amino acid means that it is necessary for the production of all the proteins in our body. You’ve heard of the importance of protein intake, and that is because proteins carry out such a wide range of functions in our body. There are antibodies (such as white blood cells), hormones, enzymes, structural proteins (such as collagen), transport/storage proteins (such as ferritin), receptors (such as Vitamin D receptors) and so many more.
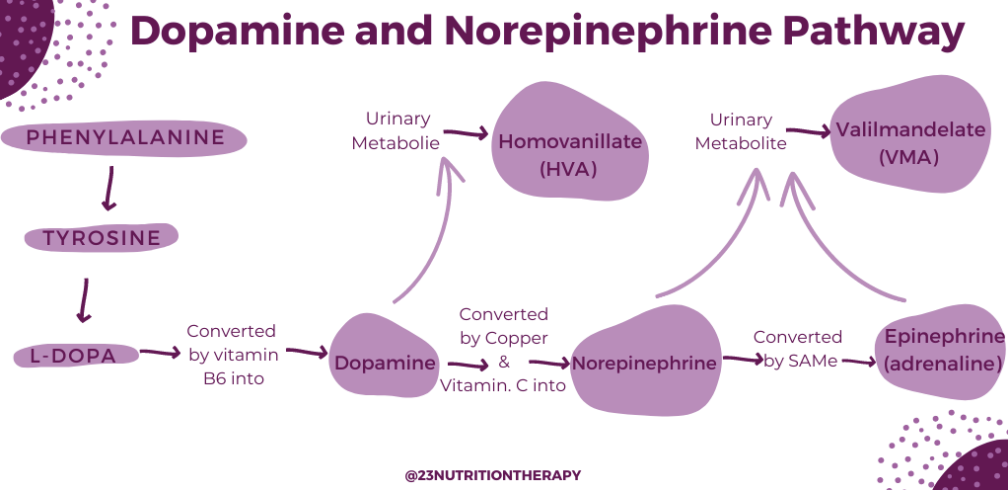
Even if we eat “the perfect diet,” our body functions still need to be in tip-top shape for us to reap the benefits of our diet. For example, you need to be able to digest, break down, and absorb nutrients, and then have the micronutrients aka precursors to support cellular pathways. Phenylalanine is a great example, our bodies convert phenylalanine into tyrosine which is then converted into dopamine through a series of intricate steps (hence why we need our bodies working optimally). Remember we need dopamine, it plays a role in our mood and allows us to find pleasure, focus, and joy. We also require phenylalanine to create norepinephrine, to support our nervous system’s response to stress.
As you may have noticed, phenylalanine is crucial for maintaining our levels of neurotransmitters in check, which helps regulate so many of our body’s functions. Protein-rich foods such as lean meats, dairy, and legumes all contain phenylalanine. Let’s continue to explore why these foods are so important to include in our diet.

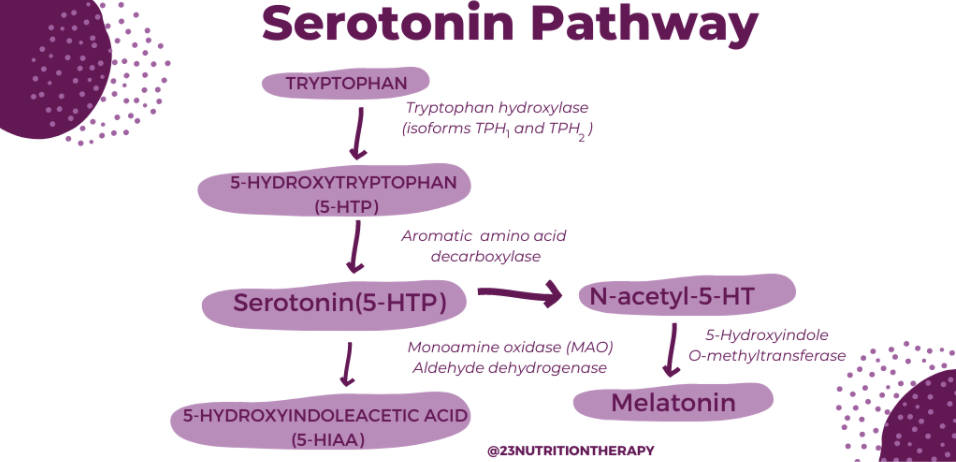
If you’ve ever felt sleepy after a holiday meal, there’s a good chance you’ve heard of tryptophan, another essential amino acid. Tryptophan is found in protein-rich foods such as turkey and chicken. Other good sources of tryptophan include legumes such as chickpeas, beans, and lentils, as well as nuts and seeds. Tryptophan is the precursor to serotonin, remember serotonin is directly tied to our sleep/wake cycles and the production of melatonin.
A high-quality protein-rich diet will supplement us with enough tryptophan to create adequate amounts of serotonin. However, a tryptophan deficiency will not only cause serotonin dysregulation but will also impact all protein functions in the body. This concept is not unique to tryptophan alone, but to all essential amino acids and nutrients, because as we’ve seen before, all of these nutrient pathways are interconnected and affect multiple body functions. If you are experiencing symptoms of anxiety, panic attacks, or sleep dysregulation, it might be beneficial to take an Organic Acids Test, which we will talk more about later.
 Now that we’ve established the importance of adequate protein intake for balancing our neurotransmitter levels, let’s take a look at the other nutrients and vitamins that are crucial for our brain health.
Now that we’ve established the importance of adequate protein intake for balancing our neurotransmitter levels, let’s take a look at the other nutrients and vitamins that are crucial for our brain health.
B vitamins are crucial precursors for building dopamine, melatonin, and other important neurotransmitters.
There are 7 different B vitamins that are important for our brain health, including vitamins B1 (thiamine), B2 (riboflavin), B3 (niacin), B5 (pantothenic acid), B6 (pyridoxine), B9 (folate), and B12 (methylcobalamin). In addition, getting adequate B vitamin intake from our food is essential for our neurological health. A deficiency of B vitamins can lead to cognitive depletion, such as sluggish thinking, impaired memory, and mood dysregulation.
Foods that are high in B vitamins include meat, organ meats, legumes, nutritional yeast, eggs, leafy green vegetables, whole grains, dairy, fruit, nuts, and seeds. The key to getting all seven B vitamins is to include a wide variety of these foods in your diet. It is important to note that vegetarians and vegans may have an especially hard time getting enough B vitamins. It’s even more important to watch those levels if you follow a plant-monogamous diet.
Omega-3 is an essential fatty acid that our bodies cannot produce, so we must get all of our Omega-3 from food. Omega-3 fatty acids are important because they help reduce and prevent inflammation in the brain and body, support cell membranes, improve immune functioning and cardiovascular health, and support our skin health. Fatty fish like mackerel, salmon, and sardines are high-quality essential sources of Omega-3. Marine algae supplements, flax seeds, and chia seeds are also adequate sources of Omega-3. To take a closer look at your omega-3 profile, an ION test might be necessary.
 Neurotransmitter Testing: Organic Acids or ION
Neurotransmitter Testing: Organic Acids or ION
Organic acids are metabolites or byproducts of cellular processes going on in our bodies. Examples of these cellular processes include energy production (think ATP and the mitochondria powerhouse of the cells), detoxification, and neurotransmitter breakdown. An Organic Acid test can give us a clue about the efficiency of these processes that are happening inside our body.
In order to get more information about your neurotransmitter levels, an Organic Acids Test can be done. This simple test involves an at-home urine collection upon waking. From there, the urine sample is sent to the lab and tested for metabolite analysis.
The Organic Acid Test (OAT) measures 46 different markers of health, including a range of different metabolites of neurotransmitters excreted by our body. The levels of these metabolites are incredibly important as they can indicate levels of certain neurotransmitters, nutrient deficiency, liver detoxification capabilities, and even bacterial overgrowth.
For more comprehensive results, an Individual Optimal Nutrition (ION) test can be done, this involves a urine sample as well as a blood draw. The ION test is similar to the OAT, but it has 125 markers. To learn more, read about ION nutritional testing here.
The results of the Organic Acids Test can provide valuable clues about health issues that may be plaguing you, such as weight issues, sleep abnormalities, and mood dysregulation. An organic acids test provides personalized results that give insight on how to better adjust your diet and supplement regimen in order to support your overall health based on your individual needs. Keep in mind that although intake may be adequate, there could be other factors at play below the surface. These can show up in the Organic Acids Test, which can be used to discover the cause of such issues.
Interested in ordering an Organic Acid Test or Individual Optimal Nutrition Test? Schedule a free consultation call!
Understanding Your Urine Test For Neurotransmitters: Neurotransmitter Balance
The Organic Acid Test or ION test will provide you with a comprehensive list of your neurotransmitter metabolite, or breakdown, levels. But it’s quite an extensive list, and it can be confusing, so what do those levels mean? Let’s find out.
Indicators of Brain Stress
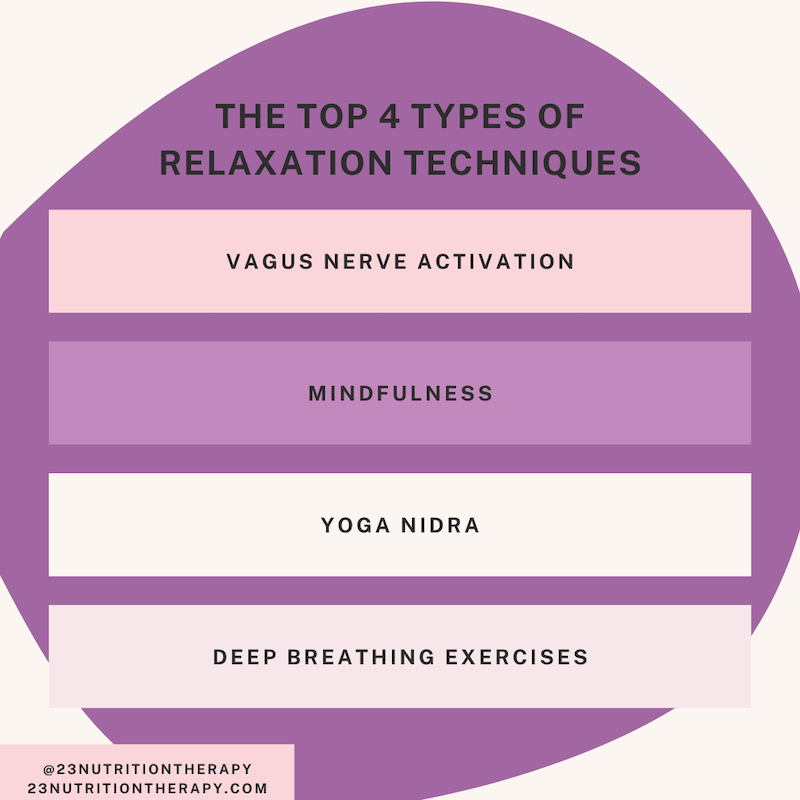
Those experiencing brain stress might be experiencing depression, anxiety, and food cravings and may greatly benefit from stress management techniques, as well as calming herbs and supplements. Some common lab values can include:
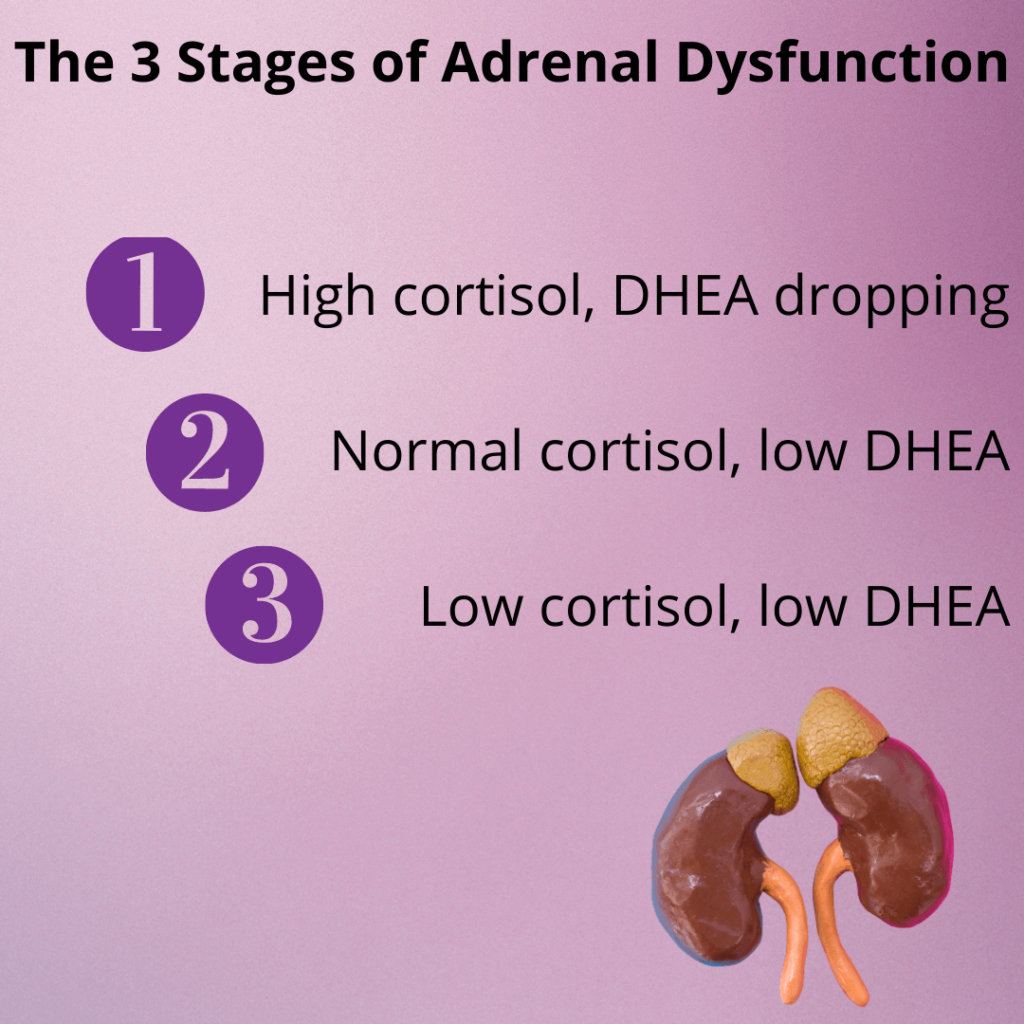
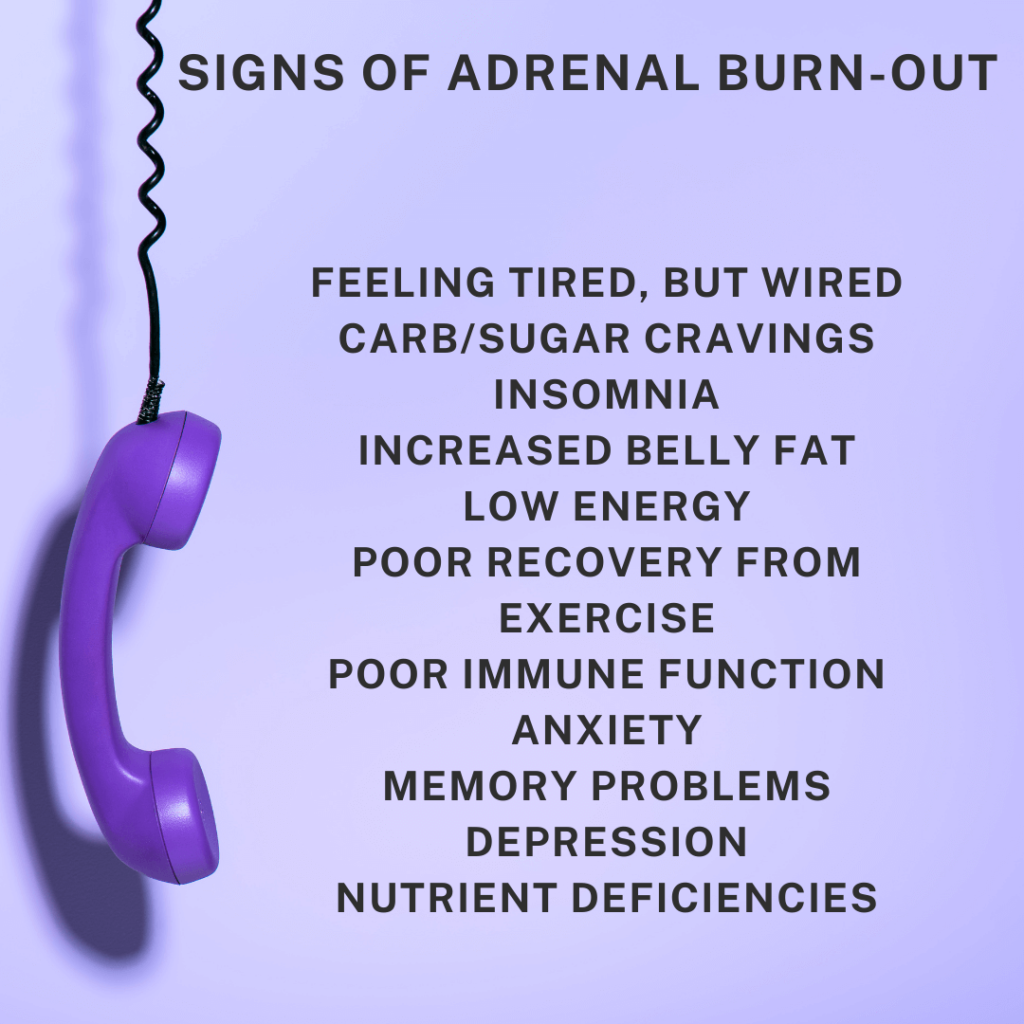
- Low HVA (Homovanillate) – Low levels of HVA can be indicative of inadequate amounts of the precursor phenylalanine or tyrosine. This can be due to inadequate protein intake or a lack of necessary vitamins required for dopamine production. Causes may include chronic stress (adrenal exhaustion), long-term antidepressant usage, inherited amino acid deficiency, many years on a vegetarian or vegan diet, or poor absorption/missing cofactors (necessary vitamins). Symptoms can include fatigue, physical exhaustion, difficulty concentrating, impulsive behaviors, loss of satisfaction, addictions, cravings, and thrill-seeking. Can be linked to Parkinsons’ and ADHD.
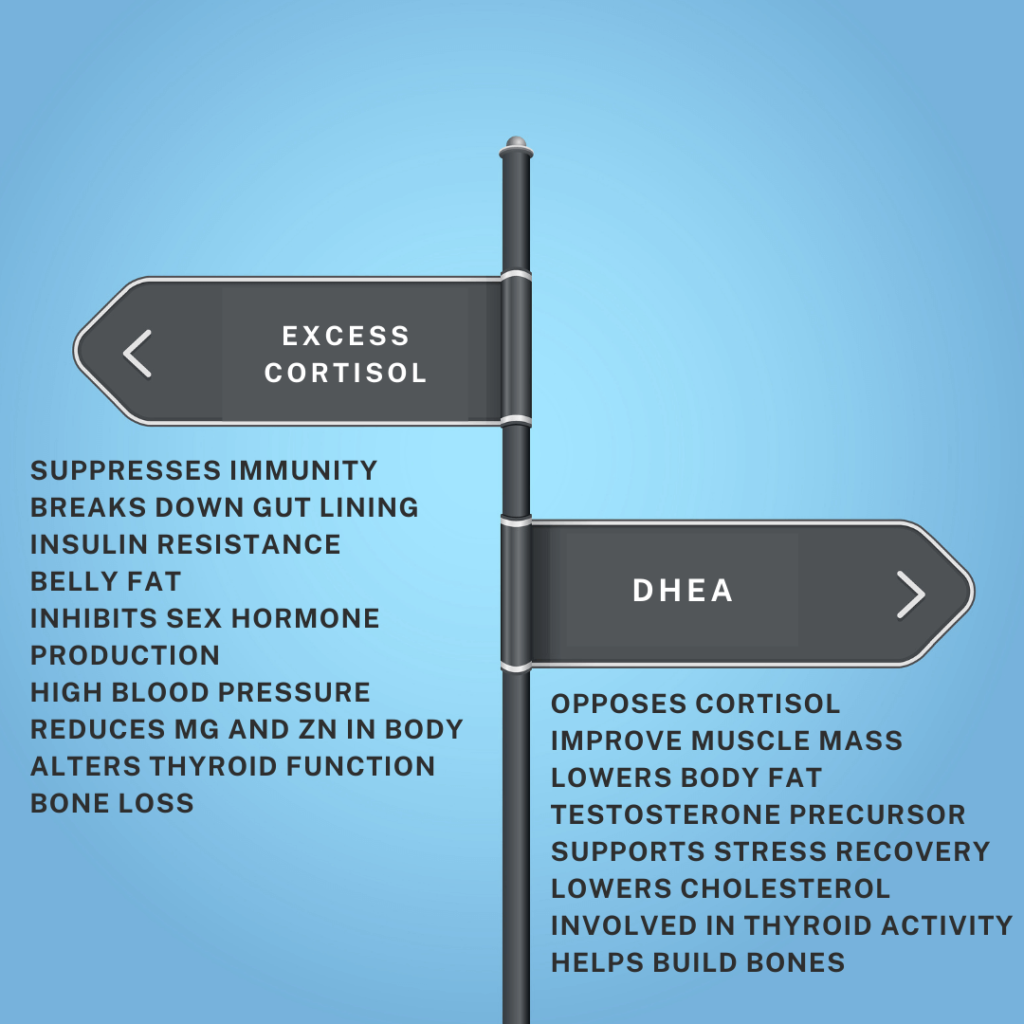
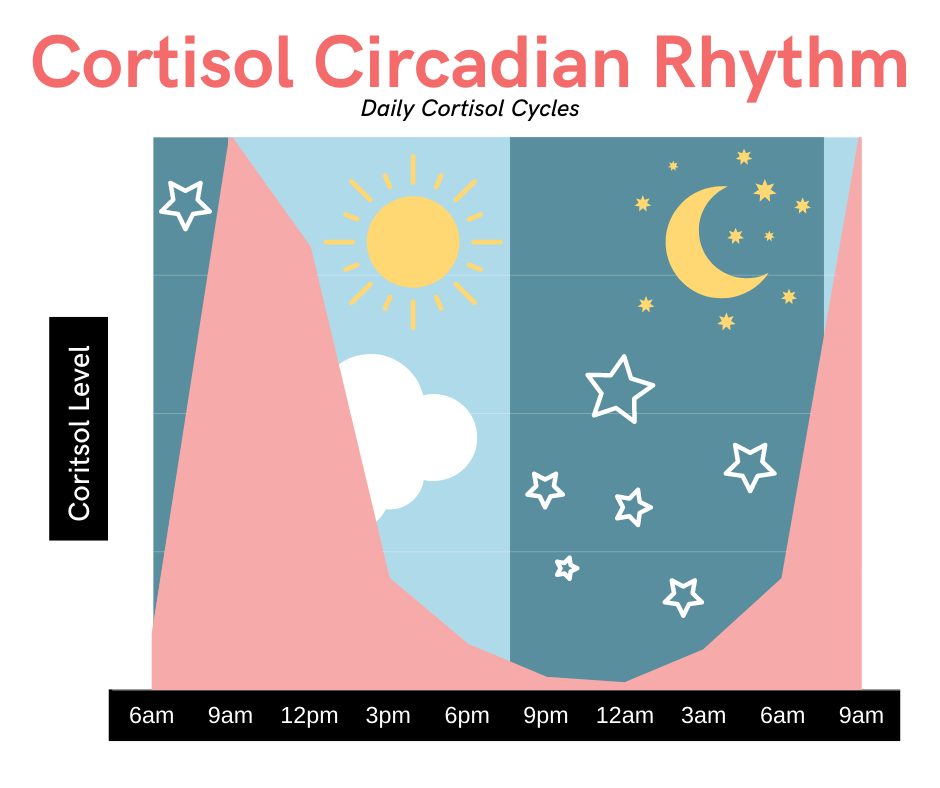
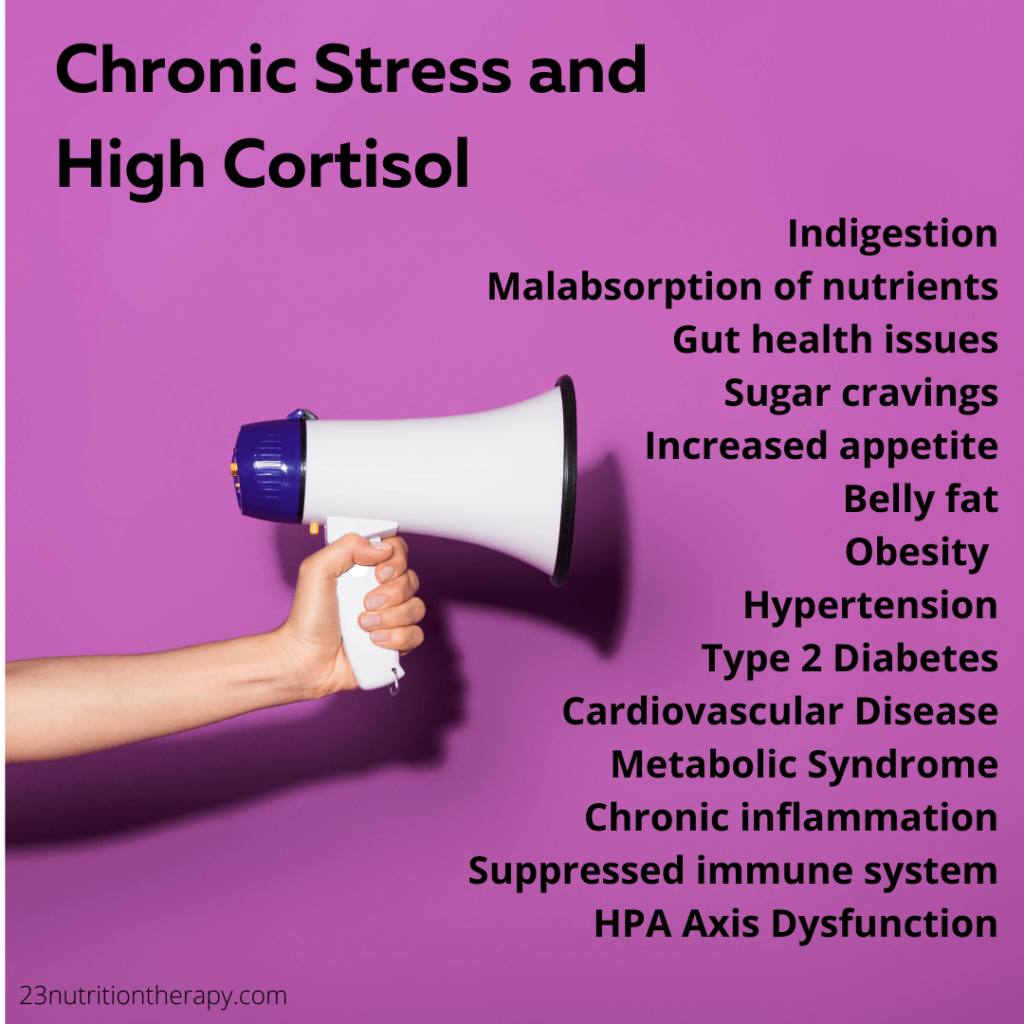
- High HVA (Homovanillate) – High HVA levels suggest that turnover rates of dopamine are too high, which can be caused by excess stress, elevated cortisol, and other stimulants such as caffeine, ephedra, pseudoephedrine, and cocaine.
- Low VMA (Vanilmandelate) – VMA is a metabolite of epinephrine and norepinephrine and when it is low, it may indicate that norepinephrine or epinephrine are not being produced at adequate levels. This can be associated with adrenal exhaustion, as well as poor protein consumption or absorption. Symptoms may include fatigue, anxiety, inability to deal with stress, sleep disturbances, and depression.
- High VMA (Vanilmandelate) – High VMA levels reflect higher than normal turnover and may indicate adrenal stress due to the overproduction of epinephrine or norepinephrine from the adrenals. This can be caused by both internal and external stressors and may feel like the nervous system is overactive. Other symptoms include headaches, anxiety, sleep disturbances, muscle aches, GI disturbances, and high blood pressure.
- Low 5-Hydroxyindoleacetate – 5-HIAA is a metabolite of serotonin and is considered to be a happy neurotransmitter. Low 5-HIAA can indicate inadequate production of serotonin. This can be caused by adrenal stress, long-term tyrosine usage, antidepressant usage, poor amino acid intake or absorption, vegan or vegetarian diets, poor absorption or missing cofactors, or inherited deficiency. Symptoms can include depression, anxiety, panic attacks, insomnia, digestive imbalances, constipation, and chronic pain.
- High 5-Hydroxyindoleacetate – High 5-HIAA may indicate a higher than normal turnover of serotonin with potential depletion of tryptophan. This can be caused by SSRI use and excess stress.
Indicators of Brain inflammation
Those experiencing brain inflammation may be experiencing nutrient deficiencies, GI inflammation, stress, and toxin-induced damage to brain cells. This can even be genetic in some cases. Let’s look at some lab-based indicators too:
- High Kynurenate – By itself, causes brain inflammation but is indicative of a B6 deficiency in the presence of high xanthurenate. Other causes of elevated kynurenate can include an inflammatory disease state and hidden stress from pathogens in the gut.
- High Quinolinate – This may make you feel flu-like. Could indicate an autoimmune disorder, IBS, parasite, or infection. This can be caused by excess inflammation and oxidative stress. Quinolinic acid can be neurotoxic in large quantities.
- High Picolinate – This can be caused by excessive protein intake and chronic inflammation.
Additionally, the organic acids test can also measure bacterial and yeast growth with 9 different markers. Bacterial and fungal overgrowth can often be found alongside many health issues. In the case of neuro-nutrition, certain types of bacterial overgrowth can prevent precursors like tyrosine and tryptophan from converting into adequate amounts of neurotransmitters.
Markers include:
- D-Arabinitol – Fungal/Yeast marker
- D-Lactate – Bacterial marker
- 3-4-Dihydroxyphenylpropionate – Clostridium Bacteria Marker
Make sure to fill out a detailed intake form which will be cross-compared to your nutritional test results to give you the best results. To learn more about bacterial overgrowth and how it affects our brain health, order a comprehensive stool analysis.
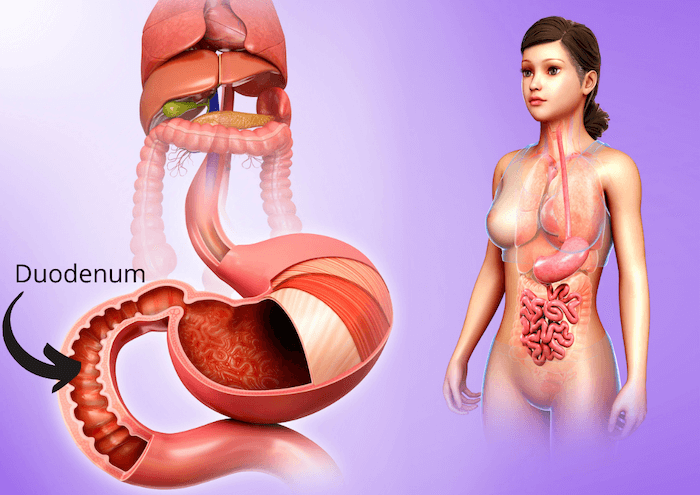
 The Gut-Brain: Gut Hormone Connection
The Gut-Brain: Gut Hormone Connection
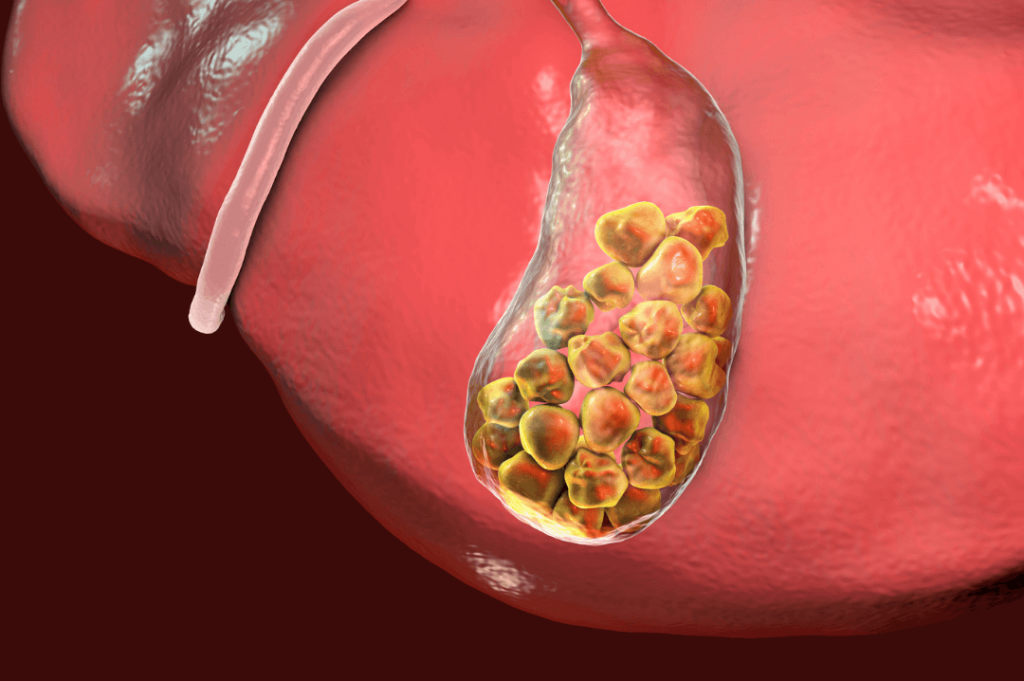
Good gut hygiene is crucial to remedy neurotransmitter imbalances. After all, if we can’t digest our food properly, none of our body systems will work at their full potential. Interestingly, around half of our dopamine is also produced in the GI tract. Somewhere around 90% of our serotonin is also found in the GI tract and there is evidence that serotonin in the gut aids in peristalsis (muscle contractions that help us digest food). So there might be more to the connection between our gut and our brain than we previously thought. Because of this, it only makes sense that if we want to keep our neural health high, we must look after our gut as well.
Some tips for keeping the gut healthy include adequate water and fiber intake to help food move. Including probiotic foods in your diet such as kimchi and yogurt can be beneficial. Limiting caffeine is also helpful in maintaining gut health. Read here to learn more about keeping your gut healthy and happy.
Some other tips for improving our neuro-nutrition include being mindful of our eating patterns, such as meal timing and blood sugar balance, making sure to eat every 3 to 4 hours, and chewing our food well so it is easier to digest. As you can see, tending to your gut health is an extremely important step to taking care of your neurological health. After all, the food we eat contains the building blocks for our brain cells! If you need a little push in the right direction in terms of neuro-nutrition, schedule a free consultation call with me.
- Resources:
- https://www.gdx.net/product/organix-comprehensive-profile-metabolic-function-test-urine
- https://courses.kalishinstitute.com/courses/enrolled/126422
- https://www.leighmerotto.com/blog/food-and-mood-nutrition-and-mental-health
- https://docs.google.com/presentation/d/1NwwkwBOpscdc-QugotcXgQiaJHkE4xX7/edit#slide=id.p20
- https://hopes.stanford.edu/about-glutamate-toxicity/
- https://pubmed.ncbi.nlm.nih.gov/31098656/
- https://www.sciencedirect.com/topics/neuroscience/phenylalanine
- https://youtu.be/C2WuzTuYYUE