How to Heal SIBO: The 3 Types
If you’re reading this, you probably know a little bit about what SIBO is and you may think that you have it. But simply thinking that you have SIBO isn’t enough to determine what happens next. The next step is to test for SIBO in order to determine if it is actually present (test, don’t guess!). And if you do have SIBO, what type of SIBO do you have? Knowing what type you have is the first step to understanding how to heal SIBO.
There are 3 general types of SIBO, which are categorized based on which gas the microbes are producing in your small intestine.
The 3 types of SIBO (small intestinal bacterial overgrowth) are:
- Hydrogen SIBO
- Methane SIBO
- Hydrogen sulfide SIBO
Each of these types of SIBO require a different approach when it comes to treatment, so knowing which kind you have is extremely important! Keep in mind; it is absolutely possible to have multiple kinds of overgrowth at the same time.
You will often see the 3 SIBO types written as “hydrogen-dominant” or “methane-dominant” because it is possible to have both but one is more dominant than the other.
How to heal SIBO completely depends on which kind or combination you have. So, staying in continuous contact with your functional medicine dietitian is vital to make sure your treatment protocol is the correct one for you!
Hydrogen SIBO

This is the most common type of SIBO. These bacteria produce hydrogen gas by fermenting carbohydrates in the digestive tract.
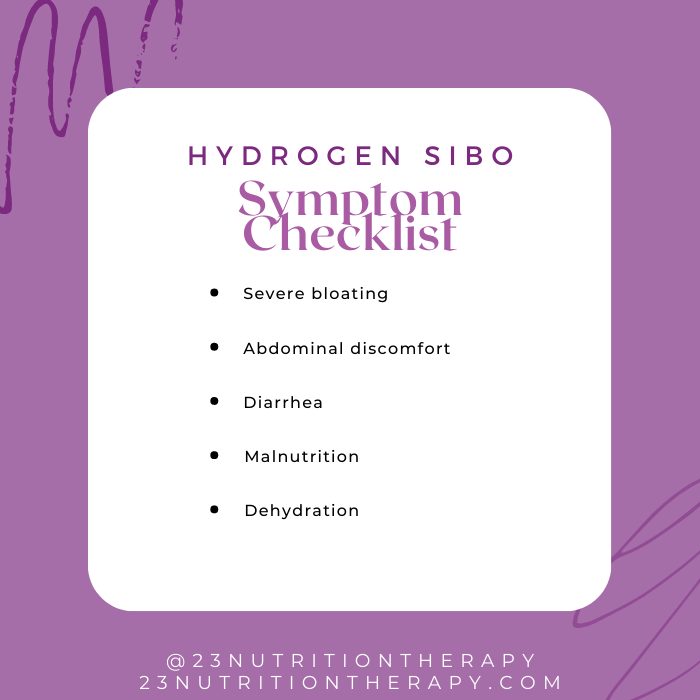
Signs and Symptoms of Hydrogen SIBO
The large amounts of gas that they produce can lead to severe bloating and abdominal discomfort, which can worsen as the day progresses.
The bacteria also produce serotonin, which increases the contractions of the small intestine. The increased frequency of contractions in the small intestine leads to a decrease in gut transit time, which results in diarrhea.
There is also another mechanism at play here that leads to faster movement through the bowels and diarrhea. Toxins released by these bacteria can irritate the gut lining, draw more water into the bowel, cause more contractions, and ultimately result in diarrhea.
It is also possible that you don’t experience diarrhea at all, and don’t experience any other symptoms.
The reduction in gut transit time also contributes to malnutrition due to the malabsorption of nutrients, because there is simply less time for the nutrients to be absorbed. The loss of liquids and electrolytes is also an issue and can lead to dehydration.
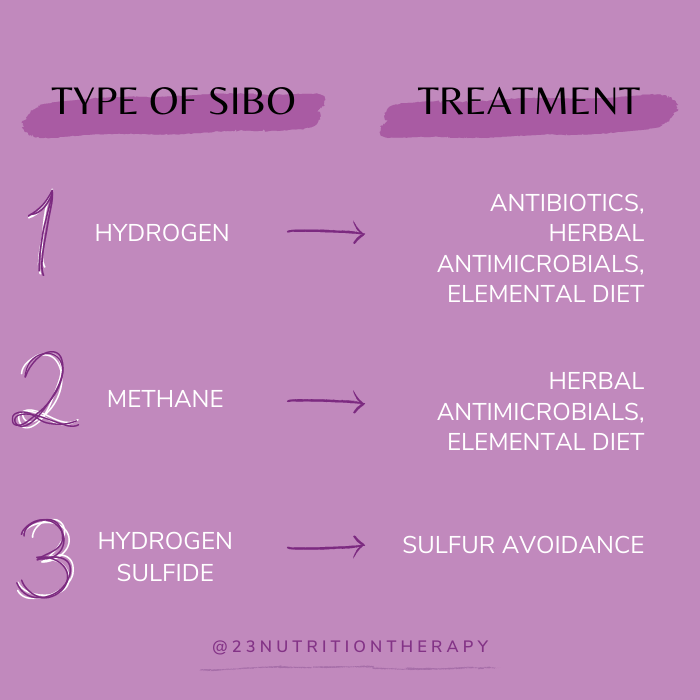
Treating Hydrogen SIBO
Hydrogen dominant SIBO responds well to antibiotics (usually rifaximin), herbal antimicrobials, and the Elemental Diet. Your functional medicine dietitian will evaluate your best course of action based on your medical history.
Methane SIBO

This type of SIBO is the second most common. Methanogens produce methane from hydrogen gas and carbon dioxide. Technically, these microbes are archaea and not actually bacteria.
There is some discussion of renaming this SIBO type to IMO (intestinal methanogen overgrowth). This name change would account for the fact that the methanogens are not bacteria. Additionally, methanogens can actually overgrow in all areas of the colon. This why SIMO (small intestinal methanogen overgrowth) isn’t the proposed name.
The potential name change highlights the fact that this SIBO type is different than the rest and requires a different approach to treatment.
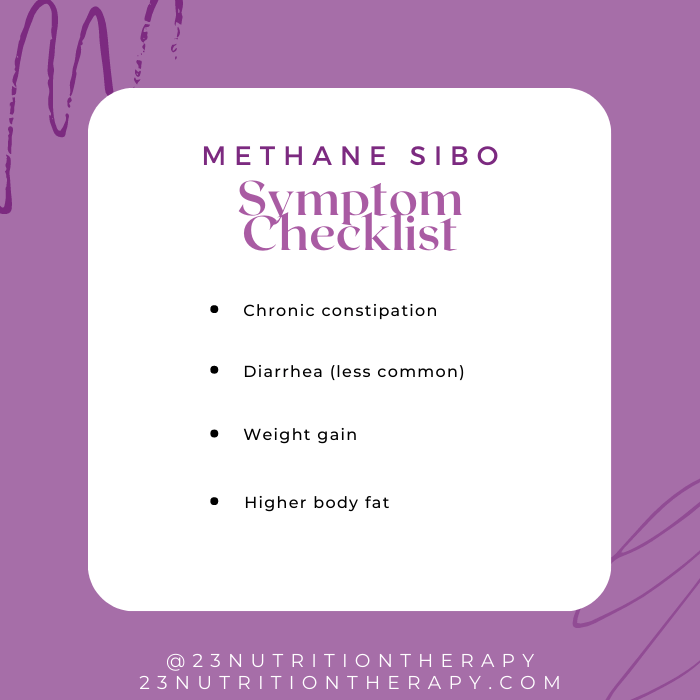
Signs and Symptoms of Methane SIBO
A common sign of an overgrowth in these archaea is chronic constipation. High amounts of methane can contribute to increased transit time within the digestive tract. The longer time food spends within the colon causes constipation. It is also possible to have diarrhea with this type, but this is less common.
Weight gain and increased body fat is also a common sign of methane dominant SIBO. This is partially due to the longer gut transit time that makes food sit in the gut for longer periods of time, allowing more calories to be extracted and absorbed.
Another reason is because archaea make more calories available to us in the gut by breaking down fiber, which we normally cannot digest by ourselves. This is the same reason cows can survive on grass alone!
Mixed Type: Methane SIBO and Hydrogen SIBO Combined
Since methanogens require hydrogen gas to produce methane, it is common to find this type of SIBO in combination with hydrogen SIBO.
It is thought that the hydrogen type can lead to an overgrowth of methanogens because it provides tons of hydrogen gas that the methanogens need! In this situation, it would be considered mixed type SIBO.
Treating Methane SIBO
Methane SIBO can be much harder to treat than hydrogen SIBO because archaea do not directly respond to antibiotics. Remember – archaea are not bacteria!
If these archaea are being fed by an overgrowth in bacteria that produce hydrogen gas, antibiotics can potentially be useful to get rid of one of the components that the archaea need. Antibiotics kill off the bacteria that produce the hydrogen gas, thus starving the archaea.
For this type of SIBO, it can be more beneficial to approach treatment with herbal antimicrobials or the Elemental Diet
Hydrogen Sulfide SIBO

This type of SIBO is a bit different from the first two. Hydrogen sulfide (H2S) is a gas that is actually produced by the human body! H2S is produced throughout the GI tract in a healthy body. In healthy levels, H2S helps to maintain the integrity of the gut lining. However, in excess amounts H2S is actually considered a neurotoxin.
With hydrogen sulfide SIBO, this normally beneficial gas is being produced in levels that are toxic! Too much H2S can lead to nerve damage, chronic gut inflammation, and DNA damage that can lead to colon cancer. The intestinal barrier can become leaky, which increases inflammation and causes other issues. Too much hydrogen sulfide can lead to immune suppression, laying the groundwork for chronic infections.
Excess hydrogen sulfide can also inhibit cellular respiration in mitochondria. Cellular respiration is the process in our cells that pulls the energy out of what we eat!
People with this type of SIBO usually feel sicker overall because of the systemic issues that result from the damage to our mitochondria. Without the ability to convert food to energy, cells can die and tissue death becomes a possibility. This also means that you aren’t receiving energy, and can result in chronic fatigue syndrome.
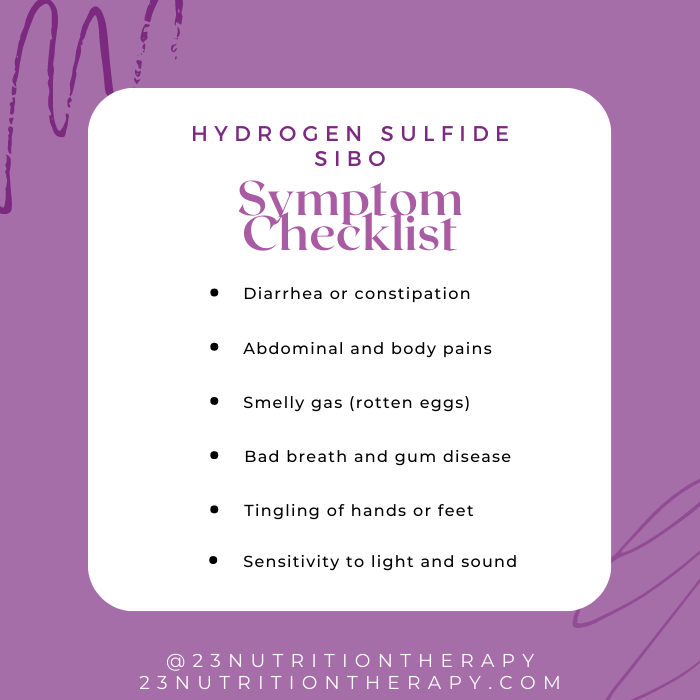
Signs and Symptoms of Hydrogen Sulfide SIBO
Diarrhea and constipation are both possible symptoms, depending on whether other types of SIBO are present. Abdominal pain and sensitivity are also extremely common. You may also experience gas that smells like sulfur, or rotten eggs. Halitosis (bad breath) and gum disease can also be the effect of excess hydrogen sulfide.
The non-GI issues that can arise due to the neurotoxic effects of hydrogen sulfide can include:
- Body pains
- Increased food sensitivity
- Tingling in hands or feet
- Sensitivity to light and sound
If you have hydrogen sulfide dominant SIBO, this doesn’t necessarily mean that you would be experiencing all of these symptoms at once.
Testing for Hydrogen Sulfide SIBO
With all of the possible issues hydrogen sulfide SIBO can cause, it is obvious how imperative it is to identify this type of SIBO. Unfortunately, this type is not currently testable by all testing methods, but that should change in the near future…
Update: there is a new test called Trio-Smart that has recently become available, and it is the only SIBO test that currently tests for all 3 types. There is some debate about whether or not this test is accurate.
There are ways for your functional medicine dietitian to make an educated guess on whether you have hydrogen sulfide SIBO from the current breath tests, but it is not a foolproof method.
About 1 in 10 SIBO cases are due to hydrogen sulfide-producing bacteria. Hopefully someday soon we will be able to test for H2S in a simple and effective way.
Treating Hydrogen Sulfide SIBO
How to heal SIBO caused by H2S-producing bacteria is different from the other types. Sulfur is needed for this gas to be produced, and we obtain that from certain amino acids in our diet. If you have this type of SIBO, avoiding foods and supplements that contain sulfur is essential for recovery.
Unlike the hydrogen and methane types, this type of SIBO cannot be treated with the Elemental Diet because the medical beverage contains these sulfur-based amino acids.
A completely different treatment approach is required for hydrogen sulfide SIBO and should be advised by your functional medicine dietitian.
The Importance of Knowing Your SIBO Type
Knowing the type of SIBO you have is extremely important. Without knowing the specific SIBO type, you will not know which type of treatment would be most beneficial. It is essential to know the type of SIBO you have to truly understand how to heal SIBO.
If you’re suffering from SIBO, you will want to pursue the most effective treatment protocol based on both your type of SIBO and your medical history, guided by your functional medicine dietitian.
Also, retesting after a SIBO treatment protocol is very important because these three types of SIBO can be interrelated. This can sometimes mean that you can get rid of one type of SIBO with the potential of having a second type remaining.
Many times you can have more than one type at once, but one type is suppressed (often the hydrogen bacteria). Hydrogen sulfide and methane both use hydrogen in order to thrive, so getting rid of either of those types might mean you’re left with hydrogen SIBO after treatment.
Now you understand why knowing your SIBO type is so important for laying the groundwork for proper treatment for healing SIBO. Working with a healthcare professional who is familiar with SIBO and who understands how to heal SIBO and all its variations will give you the best results.
Once you know which type of SIBO you have, you are one step closer to recovery! Schedule your appointment today to continue your journey to better gut health.
All About SIBO
Are you suffering from gastrointestinal distress that just won’t get better no matter what you do? It is possible that what you are experiencing is due to SIBO (small intestinal bacterial overgrowth). This would mean that you need more directed help in order to feel better!
What is SIBO?
Small intestinal bacterial overgrowth (SIBO) is a condition where the bacteria in the small intestine are growing in much larger numbers than usual.
The small intestine’s job is to absorb nutrients from the food we eat, continuing digestion after food leaves the stomach. The small intestine is the longest portion of our gastrointestinal tract, and normally contains a relatively low concentration of bacteria relative to the large intestine.
Many people generally learn that bacteria are bad or unhealthy, but the reality is that certain bacteria naturally live in our digestive tract as normal and beneficial microbiota. These beneficial bacteria help prevent other bad bacteria from colonizing and making us sick.
With SIBO, these bacteria have surpassed protective numbers and they are no longer beneficial. The bacteria have often relocated from either the mouth or the large intestine into the small bowel. Here, they start competing with you for nutrients, causing inflammation, and leading to many other health complications.
SIBO is actually a symptom of a larger problem. There are many things that can go wrong in the digestive tract that pave the way for SIBO, so what are the things that can lead to SIBO?
What causes SIBO?
Healthy digestive tracts are designed to prevent SIBO in numerous ways. The acidity of our digestive juices usually kills most bacteria in the stomach, and any remaining microbes are usually destroyed by bile in the duodenum.
The movement within the digestive tract caused by peristalsis and the migrating motor complex (MMC) prevents bacterial adhesion to the intestinal wall and sweeps materials through the digestive tract to be eliminated.
Also, the ileocecal valve blocks the passage of bacteria from the large intestine backwards into the small intestine. All of these things usually help prevent the overgrowth of bacteria in the digestive tract. So what happens when these protections fail?
Low Stomach Acid and Bile Flow
Without the proper amount of stomach acid, bacteria that would typically die in the stomach can now sneak their way into the small intestine.
Disruptions to bile flow leads to a reduction in the antibacterial nature of our digestive system, promoting small intestine bacterial growth.
The bacteria entering our small intestine can come from contaminated food or water. They could even be the bacteria that naturally live in the mouth. Sometimes these bacteria are detrimental to our health; secreting toxins that trigger food poisoning with extremely uncomfortable symptoms, inflammation, and can even lead to the paralysis of the MMC.
MMC Dysfunction
The job of the MMC is to sweep undigested food and bacteria through the digestive tract between meals.
When the MMC malfunctions, bacteria hang out in the small intestine long enough to flourish, a root cause of SIBO. Anything that leads to the dysfunction of the MMC can cause SIBO because the housekeeping isn’t taking place, leaving food in the small bowel for bacteria to thrive on.
Surgery
SIBO can also be a consequence of gastric or abdominal surgeries, constipation, or anatomical structural abnormalities that cause obstructions in the intestines.
Blockages further in the system can lead to bacteria from the large intestine migrating upward through the GI tract and ultimately translocating into the small intestine where they don’t belong.
Chronic Stress

An overarching root cause of SIBO can actually be stress, which leads to issues with the gut-brain connection. The underappreciated vagus nerve connects our mind and digestive system, sending signals from digestive organs to the brain and vice versa. This nerve innervates nearly every organ in our torso, supplying them with parasympathetic, rest and digest impulses.
Stress inhibits the vagus nerve, leading to the sympathetic, fight or flight responses predominating. Digestion is halted during stressful situations, because energy is needed elsewhere in the body in preparation to escape or battle a potential threat.
When digestion is halted, less stomach acid is produced. Another consequence is that the MMC will shut down, leading to the stasis of food and bacteria in our system. It all comes together… stress can cause the problems that lead to SIBO!
The connection between our gut and brain is bidirectional: the situation in our gut impacts our brain, and the situation in our brain influences our gut.
This can turn into an unrelenting cycle where you start off stressed, then your gut starts acting up, then you become even more stressed due to the gut issues, which never improve because you’re stressed out! Yikes, deep breaths…
Signs of SIBO

Symptoms of SIBO include:
- Gas
- Bloating
- Diarrhea
- Constipation
- Acid reflux
- Nausea
- Abdominal cramps
- Leaky gut
- Migraines
- Depression
- Anxiety
- Brain fog
- Fatigue
- Eczema
Other signs to watch out for are the outcomes of malabsorption: anemia, weight loss, and certain nutrient deficiencies.
SIBO co-occurs with many other conditions including:
- IBS
- Leaky gut
- Celiac disease
- Ulcerative colitis
- Crohn’s disease
- Hypothyroidism
- Fibromyalgia
According to the SIBO Academy, around 1 in 5 adults in the United States have IBS – and over 1/3 of these cases also have SIBO. There is also a high correlation between SIBO and NAFLD (non-alcoholic fatty liver disease) due to the accumulation of bacterial toxins that cause inflammation.
Since SIBO can present with a wide variety of symptoms and comorbidities, both GI and non-GI, it can often be difficult to identify based on symptoms alone. The non-GI symptoms are neurological and psychological, resulting from dysfunction in the gut-brain connection. It is important to take note of and communicate any symptoms you experience.
Identifying SIBO requires a comprehensive overview of your medical history including reviewing medications, assessing risk factors, evaluating diet and nutrient levels, and of course, a sibo test.
Testing for SIBO
SIBO can be detected through hydrogen and methane breath tests, which measure the production of these gases within your digestive system.
The SIBO breath test involves drinking a sugar solution containing either glucose or lactulose, and then periodically blowing into a tube to measure the amounts of gas present over time. Blowing into the tube at specific intervals over a period time is important because the timing is what indicates the location in your digestive tract where these gases are being produced.
Breath tests are valuable because our bodies don’t produce these gases – the bacteria do. Bacteria thrive on carbohydrates for energy by fermenting sugars and producing methane or hydrogen gas as a result. In healthy people, the bacteria of the large intestine are exclusively responsible for this gas formation.
With SIBO, the small intestine bacteria also end up producing these gases. Elevated levels of these gases within a certain timeframe of the test can expose the presence of SIBO, suggesting a decreased ability for your body to absorb nutrients and signaling to other potential issues.
There are 3 types of SIBO, dependent on which gas is being produced:
- Hydrogen
- Methane
- Hydrogen sulfide
It is possible to have more than one type of SIBO present at once, especially methane- and hydrogen-dominant types. Unfortunately, there is not a test available for hydrogen sulfide SIBO yet, but that could change in the near future. (There is now a H2S test, but it has not been recommended by professionals yet)
Healing SIBO
Treating SIBO is crucial because without intervention, the negative symptoms will persist. This can lead to malnutrition resulting from the decreased absorption of nutrients.
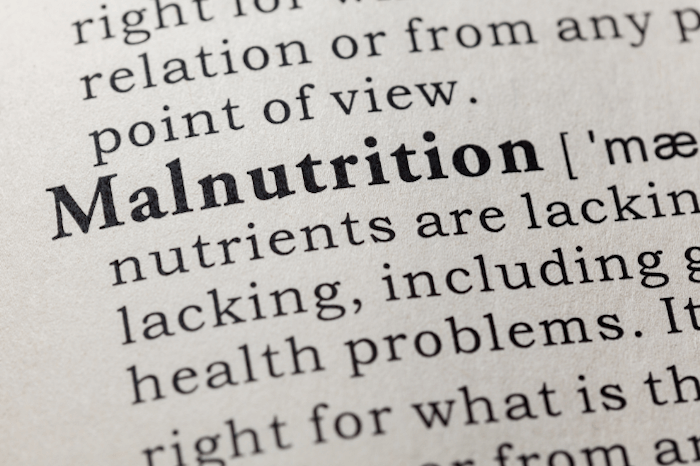
SIBO can lead to nutrient deficiencies of iron, fat-soluble vitamins (A, D, E, K), vitamin B12, and calcium. SIBO can also prevent absorption of macronutrients: proteins, fats, and especially carbohydrates. Deficiencies in any of these nutrients can lead to other complications that can negatively impact your health.
Antibiotics can be used to treat SIBO by killing and removing bacteria from the gut. Initially, this may sound like exactly what we need, but remember that a certain amount of gut bacteria is actually favorable.
SIBO is not an infection and will not respond to treatment the same way infections do. Antibiotics kill both the overgrowth and the beneficial bacteria that aid in digestion. About half of the time, antibiotics for SIBO will return due to the fact that one’s diet and lifestyle often need to be adjusted in order to prevent recurrence.
The most effective approach to treating SIBO and maintaining a healthy gut post-intervention is to utilize the 5R protocol which addresses more than just the removal of the bacterial overgrowth.
The 5R Protocol is an all-encompassing approach that directs attention to all of the factors that can impact recovery.
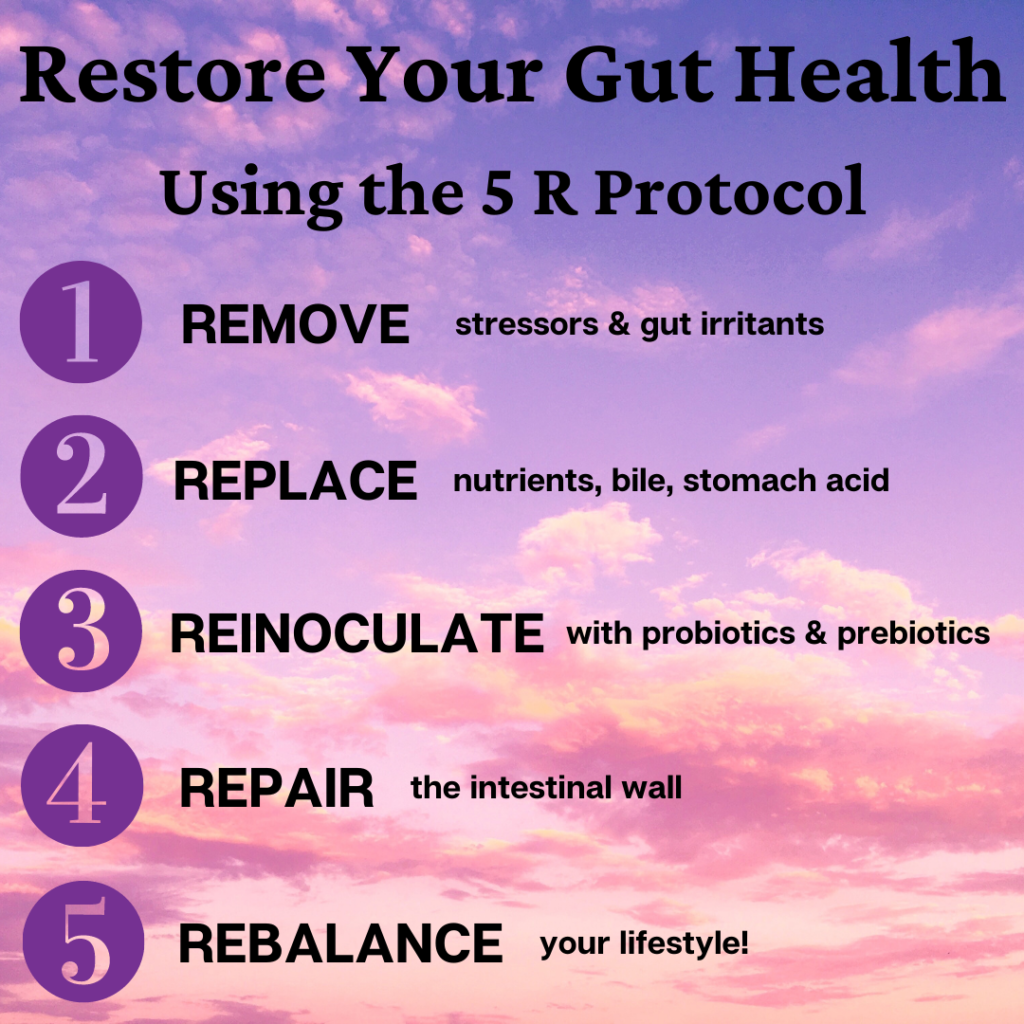
- Remove excess bacteria by removing stressors and irritants
- Replace bacteria using digestive enzymes
- Repopulate using probiotics and prebiotics
- Repair the intestinal wall with nutrients and supplements
- Rebalance lifestyle to support maintenance of a healthy gut
Best Diet for SIBO

Getting rid of the bacterial overgrowth is the first priority, so how do we accomplish that? Many of the diets for SIBO that may be recommended to starve the bacteria can be stressful to follow, difficult to understand, and time consuming. These diets can be extremely restrictive, leading to orthorexia (food obsession) or even further nutritional deficiencies.
There is one diet for SIBO that is easy to follow. It effectively starves the bacteria in just 2 ½ to 3 weeks all while still providing adequate nutrition to the body. This diet for SIBO is called the Elemental Diet. Following this diet for SIBO requires consuming only a medical, complete-nutrition beverage for 2 ½ to 3 weeks.
This diet can be just as effective as herbal or antibiotic interventions. This makes it a great option for those with stubborn cases or those who want quick results. It is similar to fasting, so social support along with constant contact with your dietitian is essential to ensure lasting results.
After completing the Elemental Diet intervention to remove SIBO, the rest of the 5R protocol should be followed in order to sustain gut healing and prevent relapse.
In the same way that gut health issues don’t appear overnight, SIBO won’t vanish overnight. But with a little time and effort, you can heal your gut microbiome and go back to living your life with less stress, less discomfort, and improved wellbeing!
Do you think you have SIBO? Instead of sitting in doubt, make an appointment today to take the next step to improve your gut health!

