There is so much information on the Internet about how to improve gut health and relieve uncomfortable symptoms. It can be confusing to know where to begin if you’re doing the research on your own. Do I need to take any supplements? How about probiotics? Should I avoid certain foods? Should I get tested for – insert any of the multitude of gut conditions here? How do you really find out what is best for you to heal your gut?
Unfortunately, there is not a “one size fits all” answer when it comes to gut health. The types of things listed above should always be done in coordination with a dietitian, who has the knowledge to guide you in the right direction according to your personal needs.
The good news is that there are some easy gut health lifestyle changes that you can start doing today that can help lay the foundation for a healthy gut!
Here are 5 simple lifestyle changes you can make that will help you to heal your gut!
1. Slow down while eating
Are you the type of person who rushes through their lunch break? Or maybe you’re finished with your meals within a mere 10 minutes. Please stop eating food too quickly! It is important to chew your food sufficiently in order to heal your gut.
Chewing is an essential part of digestion. Chemicals in our saliva, such as digestive enzymes, help us break down certain nutrients. The antimicrobial properties of our saliva also help to kill some potentially pathogenic bacteria that may be present in the things we consume.
Chewing until food is soft and smooth makes digestion easier further down the digestive tract. Not chewing food enough may lead to digestive problems, malnutrition, and dehydration. Bloating, diarrhea, acid reflux, maldigestion, gas, and abdominal cramping can all result from not chewing your food enough.
Mindfulness and eating go hand in hand because it promotes the parasympathetic, rest and digest state. This is the state you need to be in for the digestive processes to kick in and do their job. Avoid stress during meal times, and try to eat slowly to really enjoy your food. This should lead to better digestion and nutrient absorption.

How to slow down while eating:
- Chew your food about 30 times before swallowing.
- Aim to swallow only a couple of times per minute.
- Make mealtimes relaxing and practice mindfulness
2. Quit snacking
Spacing out meals is really critical for gut health. We need to have periods of time without food in our system in order for the migrating motor complex (MMC) to fulfill its housekeeping duties.
The MMC is responsible for flushing out undigested materials and bacteria through our digestive tract to eventually be flushed down the toilet. If the MMC cannot do its job, bacteria in the gut now have a chance to overgrow by thriving off of the undigested materials that continue to hang out in the gut. Repeatedly stalling the MMC can lead to conditions like SIBO (small intestine bacterial overgrowth), which can lead to many other digestive and systemic issues.
A general rule is to wait about 3 to 4 hours after a meal before eating again. This should ensure that your MMC can serve its purpose, leaving a clean slate for your next meal. Getting your MMC functioning optimally is essential to heal your gut.

Another perfect time for the MMC to perform its housekeeping duties is while you’re asleep! Sometimes that midnight snack sounds really appealing, but our digestive functions work best if given a 12-hour overnight break. So be sure to make your meals count: they should be nutritious, balanced, and keep you full until your next meal.
How to stop mindless snacking:
- Eat balanced meals containing protein, healthy fats, and complex, fiber-rich carbs with sufficient calories that will keep you fuller for longer
- Meals should be spaced out about 3 to 4 hours
- Don’t eat between dinner and breakfast for a 12-hour overnight fast
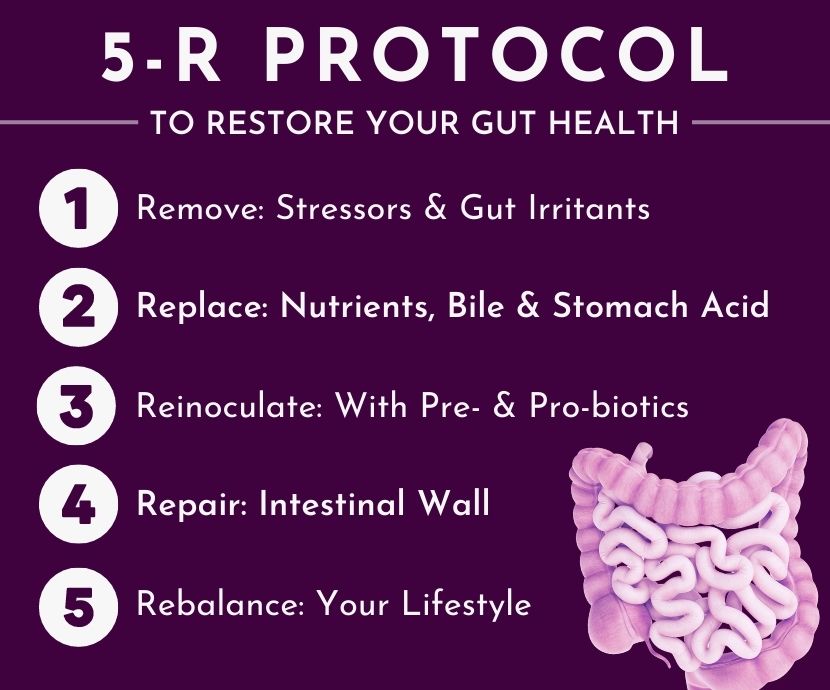
3. Remove stressors from your daily life
Stress negatively impacts many aspects of our overall gut health. Most people are familiar with experiencing digestive issues when going through stressful situations such as job interviews, a big exam, or a presentation at work.

Spending more time doing the things you love, and less time doing things that stress you out is an easy way to elevate your overall health. Not only will you feel happier… you will also become healthier and each of these leads to an overall increased sense of wellbeing. Healing your lifestyle can directly lead to you being able to heal your gut.
Keep track of the moments when you feel stressed and find the patterns. There may be some things you’re able to remove completely.
- Maybe your home environment is cluttered and messy?
- What if you have a toxic relationship with social media?
- Maybe your email inbox is at 13,000 unread emails?
- Perhaps you’re always running late?
- Maybe you tend to procrastinate?
These are all situations that can be avoided and removed.
- Clean your house to help declutter your mind.
- Take a weekly social media hiatus and spend the time you gain back on a hobby.
- Break up the big task of going through 13,000 emails into smaller increments, scattered throughout the week.
- Leave earlier for work, appointments, and plans with friends.
- Use time-blocking to organize your time better, leaving no room for procrastination.
Doing the work to remove the stressors that are under your control can put you on the path to better overall health.
Sometimes the things that stress us out are out of our control. If it isn’t possible to completely remove certain stressors, the next best thing would be to improve your response to stress.
4. Practice mindfulness and relaxation techniques
Relaxation techniques that are successful in improving gut health outcomes include things like: deep breathing exercises, mindfulness, meditation, and yoga.
Square breathing (AKA 4×4 breathing, block breathing) during a stressful event is an effective way to help pull your focus off of the negative feelings and elicit a state of calm within the body. To do this, inhale for 4 seconds, and then hold for 4 seconds. Next, you exhale for 4 seconds, and then hold for 4 seconds. Repeat this cycle until you feel more zen and less stressed. It is important to note that when you inhale, your belly should expand rather than your chest.
Mind-body practices like mindfulness, meditation, and yoga have been shown to reduce perceived stress and help regulate stress response systems. Mindfulness involves being more aware and conscious in the present moment.

This can be done by tuning into bodily sensations, paying detailed attention to your surroundings, and allowing thoughts to come and go without judgment. Mindfulness is a form of meditation that can easily be performed any time or place. Yoga, mindfulness, and meditation (in the classic, more formal sense) can all improve your reactions to stressors over time.
Using whichever relaxation technique that best works for you can help heal your gut and improve your overall well being. Being able to respond more calmly to stressful situations comes with practice, and this ability is directly related to the function of a very special nerve in your body: the vagus nerve.
5. Improve your vagal tone
The vagus nerve is often under-appreciated. It relays signals between the brain and almost every organ in your torso, however it works best when we are in an unstressed state. This is the reason why digestion doesn’t work properly when you’re stressed out! The vagus nerve creates what we call the gut-brain connection.
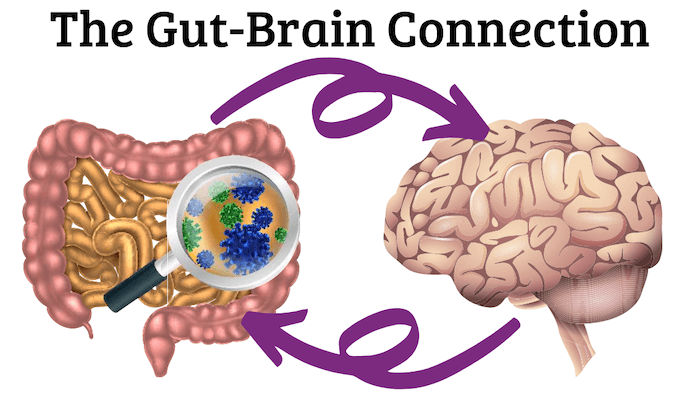
Many people live with chronic stress which directly impacts gut function. This chronic stress can lead to poor vagus nerve function, but there are measures we can take to stimulate the vagus nerve and have an increased vagal tone. Increased vagal tone indicates that you can relax quickly after you experience stress.
Stimulating the vagus nerve can be done in several different ways, and can lead to the dampening of the stress response, putting you in a state of relaxation. A couple of the easiest ways to stimulate the vagus nerve are possible due to the fact that the nerve runs through the muscles in the back of the throat.
One of these simple exercises includes humming or singing at the top of your lungs while showering or driving to work. Gargling warm salt water for 30 seconds (until your eyes begin to water) will also activate the vagus nerve.
Practicing vagus nerve stimulation can serve to modulate your body’s automatic stress responses, and over time you may actually find yourself more capable of remaining calm and stress-free. Tuning in to your body and being mindful of how you respond to stress — and noting how often you feel stress — is the first step in improving how your body reacts.
Now you have a few more tools in your toolkit that will help you to heal your gut!
Always pay attention to your body and trust your gut! Never be afraid to ask for help.
For personalized guidance for how to achieve a healthy gut, schedule your appointment today!