What is IBS?
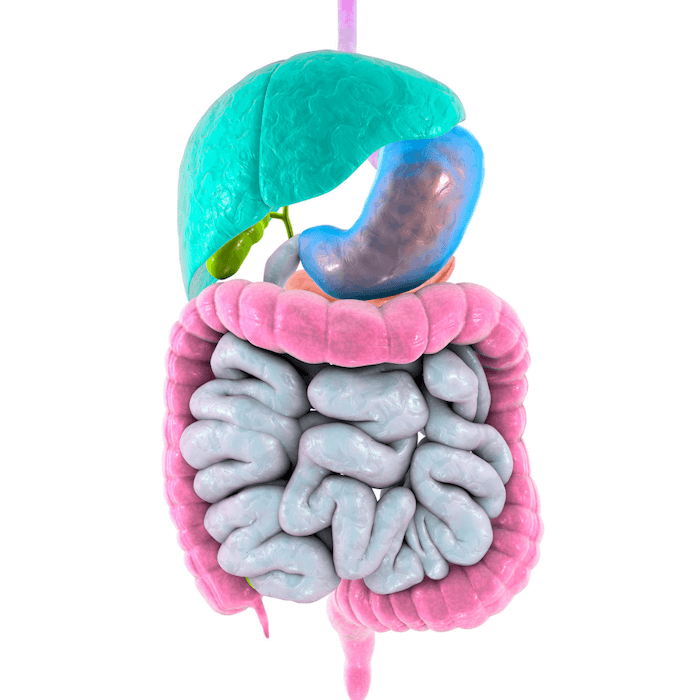
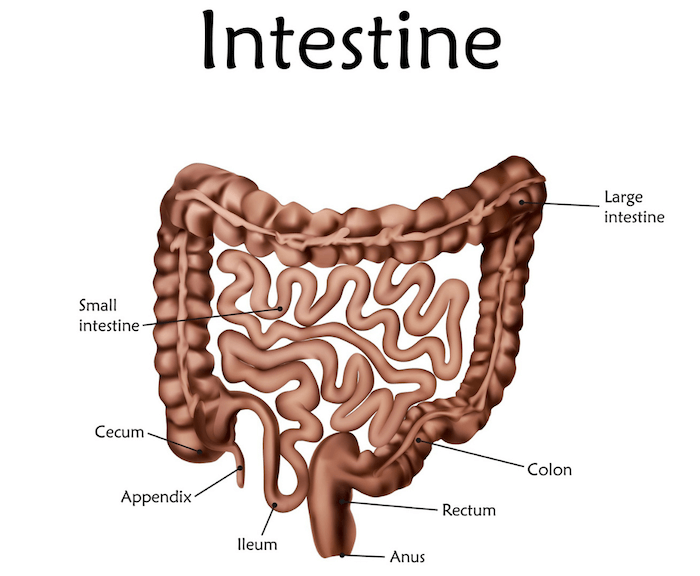
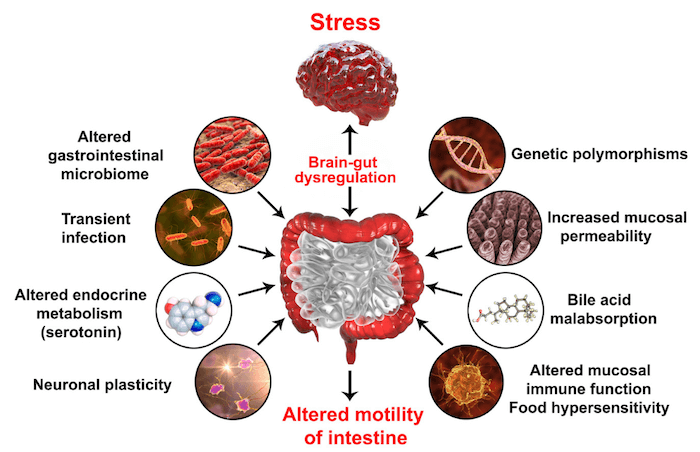
IBS stands for Irritable Bowel Syndrome, a fairly common disorder that affects the gut, including the stomach and the intestines. It is an umbrella term for a group of symptoms that affect the gastrointestinal tract which otherwise might not have an obvious etiology or cause. It is essential to note the difference between IBS and IBD, inflammatory bowel disease is a chronic autoimmune disease that includes intestinal swelling. There are many potential root causes for IBS and many factors that play into these root causes.
Let’s first talk about the symptoms of IBS and take a deeper look into the root causes and treatments.
Symptoms of IBS – Understanding IBS Signs and Symptoms
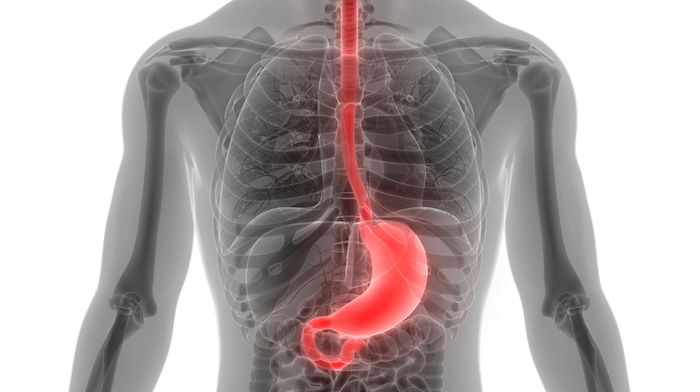
IBS symptoms are easily overlooked. The main symptoms of IBS include abdominal pain and/or discomfort along with recurrent or consistent diarrhea, constipation, or overall change in bowel habits. Another common symptom is bloating after eating or feeling like you cannot fully empty yourself. Other symptoms that often go along with IBS include acid reflux, genitourinary symptoms, headaches, backaches, brain fog, and anxiety. GERD, gastroesophageal reflux disease is also common for those with IBS symptoms, including acid reflux flare-up episodes.
Types of IBS – Understanding Different Kinds of IBS and Diagnostic Criteria
IBS is generally categorized into 2 to 3 subcategories: IBS-C, IBS-D, and IBS-M. While they all share some similar symptoms, IBS-C most common symptom is constipation, IBS-D most common symptom is diarrhea, and IBS-M most common symptom is a mix of diarrhea and constipation.
One diagnostic method for IBS is the Rome criteria. The Rome criteria was initially released in 1994 but has been updated periodically as science has evolved. The Rome IV criteria from 2016 include recurrent abdominal pain for at least 1 day/week on average in the last 3 months as well symptoms related to defecation, change in frequency of stool, and change in form/appearance of stool. If this sounds like you, keep reading to find out more about IBS and see how we can work together to find the root cause and alleviate your symptoms!
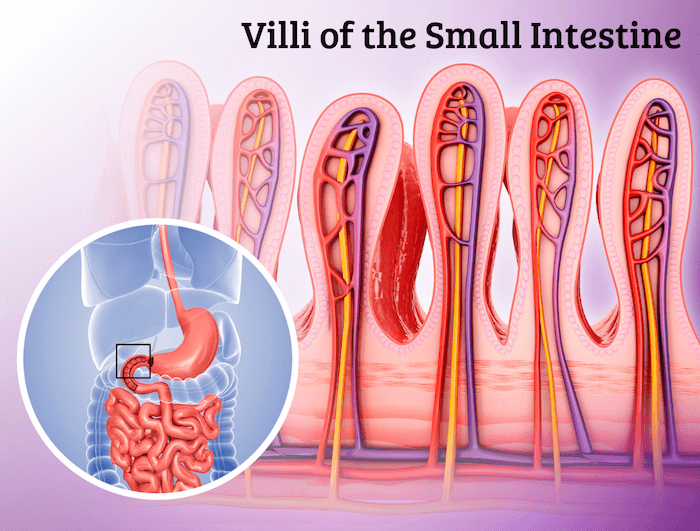
While the research is still new, IBS has been associated with leaky gut syndrome, which is defined by an increase in intestinal permeability concurrent with gut-associated membranes/tissues. Your small intestinal lining is considered semi-permeable meaning that under normal circumstances, it should allow for nutrients from food to be absorbed into the bloodstream while containing/blocking the absorption of undigested foods, toxins, bacteria, and pathogens from being absorbed. If this lining is compromised, these larger particles, bacteria, toxins, etc… are absorbed into the bloodstream causing an immune response and systemic inflammatory reactions throughout the body.
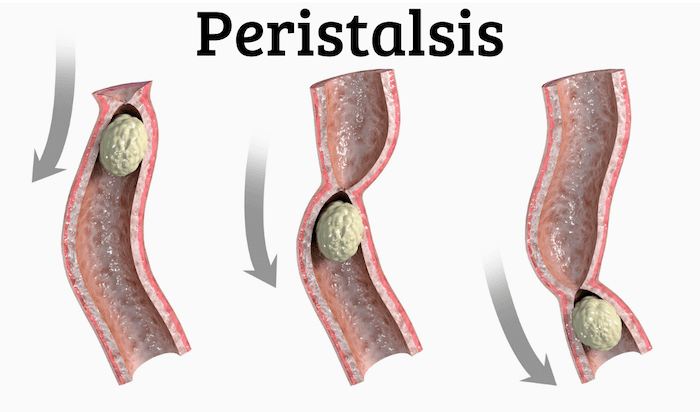
Another potential cause of IBS is post-infectious IBS (PI-IBS). Gut infections like gastroenteritis AKA food poisoning or Giardia can cause PI-IBS. PI-IBS should not be ignored as it can cause damage to the vagus nerve and affect intestinal motility. These combined can also lead to SIBO. The symptoms of PI-IBS are similar to that of IBS-D we discussed. PI-IBS can actually be tested by testing antibodies called anti-CdtB and anti-vinculin. These antibodies are produced if the body believes it needs to fight against them or if there is bacterial overgrowth. Testing can also tell us if IBS is related to a small intestine bacterial overgrowth, SIBO.
Root Causes for IBS
As we’ve already seen, IBS is a sort of blanket diagnosis because there are so many potential things happening at once with similar symptoms. There are many potential root causes for IBS. Let’s dive in!
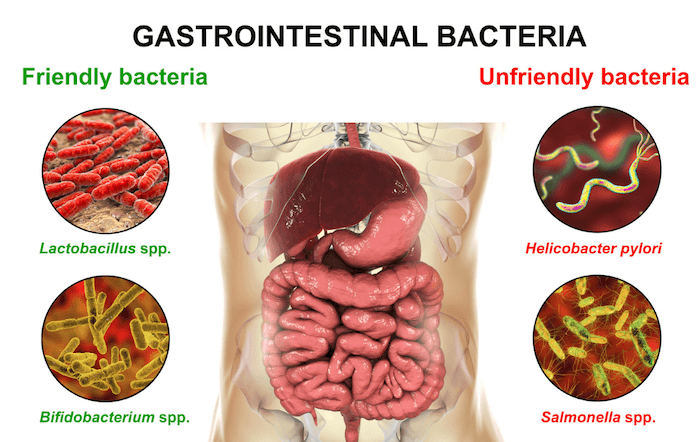
Can H. pylori Lead To IBS?
H. pylori, also known as helicobacter pylori, is a bacterium generally found in the stomach. While normally asymptomatic, H. pylori can cause inflammation of the stomach causing gastrointestinal symptoms. While it is estimated that over 50% of the world has H. pylori, new research shows that H. pylori may promote the development of IBS and as such should be tested and treated accordingly. As we have already discussed with H. pylori, infections of the gut can cause IBS symptoms to flare up. Other infections include opportunistic bacterial infections such as yeast infections and parasitic infections that can lead to a dysbiosis of the gut and can ultimately result in a flare-up of IBS symptoms.
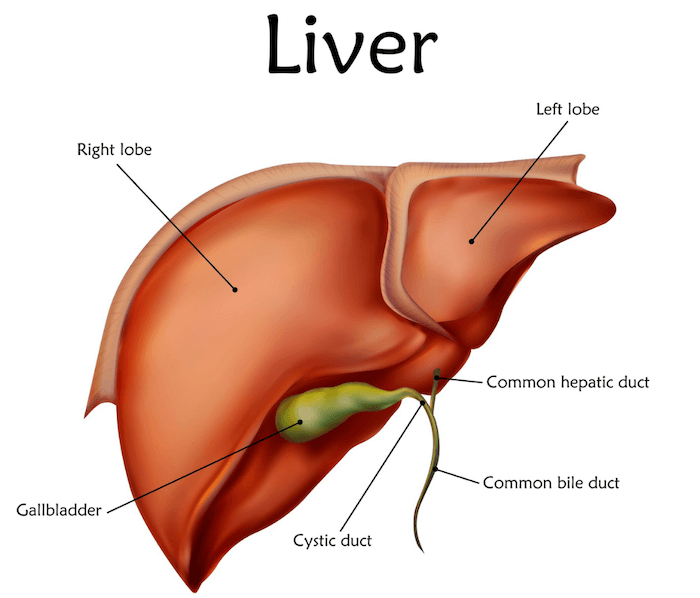
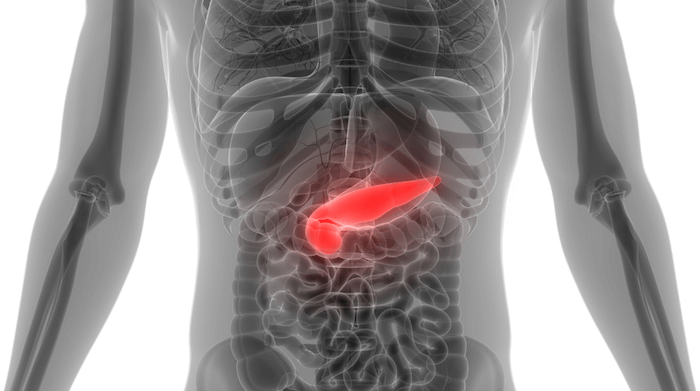
Enzymes: Pancreatic, Stomach Acid, Bile Acid
The pancreas is both an endocrine organ (meaning it produces hormones) and an exocrine organ. The exocrine functions of the pancreas include producing and releasing digestive enzymes. Digestive enzymes play a key role in breaking down the food we eat for the body to absorb. Issues with the pancreas that result in a lower production of these enzymes can be categorized as a type of IBS and maldigestion.
Low enzyme symptoms aside from general IBS symptoms can also include food in the stool and sticky stool. While these symptoms may seem like “your normal”, do not be fooled, these are not normal and the root cause must be discovered to create long-lasting relief.
These are also important as they can be root causes of SIBO too. Increased fecal fat levels, also called steatorrhea and a result of low enzyme levels and maldigestion/malabsorption, can increase the risk of SIBO as well and should be noted as a contradiction for certain diets like KETO which are high in fat. Working with a functional medicine dietitian to find the right balanced diet is key.
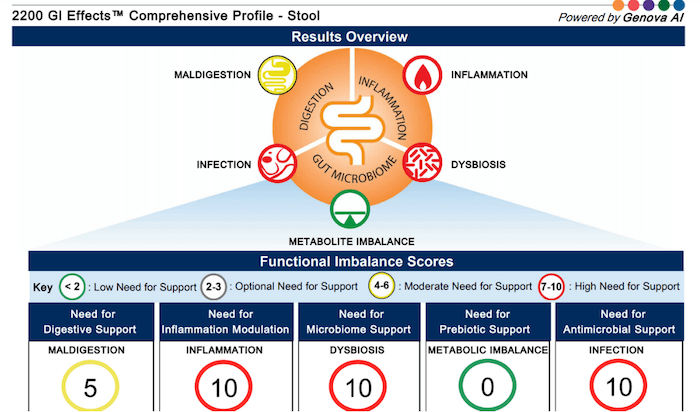
As we talked about before, GERD (acid reflux) is a common symptom of IBS all relating back to stomach and bile acid. Bile acid has recently been researched more specifically in relation to IBS-D as bile acid can mitigate bowel function and is closely connected with the gut microbiota. This is another reason why proper testing is so crucial in our diagnostic process. One of the things that the GI-Effects stool test specifically looks at, unlike the standard GI Map, is fecal fats in the stool which tells us about the need for bile acids. Despite the GI-Effects being the less commonly run test, it actually dives deeper in helping us find the root cause of your digestive issues.

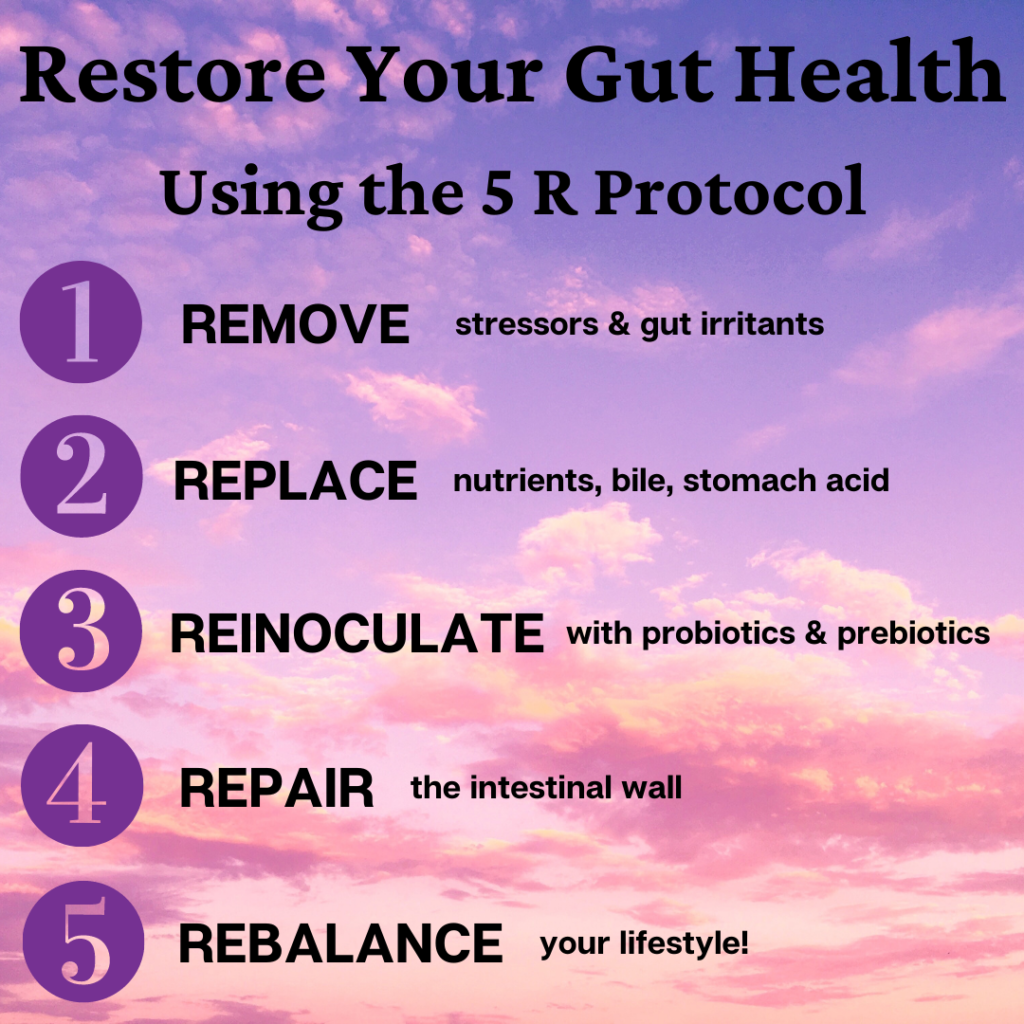
Digestive Enzymes vs. Probiotics
Let’s talk about the difference between digestive enzymes and probiotics. Digestive enzymes are secreted by different exocrine glands like the salivary glands, the gastric glands, and by types of cells in the pancreas and small intestine. Digestive enzymes are what break down the larger macromolecules of our foods like fatty acids, carbohydrates, and proteins, for example, into smaller molecules that our body can then absorb and use accordingly.
Probiotics, on the other hand, are live microorganisms that help to improve/restore your natural gut microbiota. In the same realm, prebiotics are essentially what feed the probiotic microorganisms in your gut to maintain a healthy gut microbiota.
Both pre- and probiotics can be acquired through your diet and while digestive enzymes are typically produced by our bodies, sometimes we need more support through proper supplementation.
Working with a functional medicine dietitian to get proper testing and curate a proper regimen is key to maintaining a healthy gut microbiome if you suffer from digestive issues.
Low Secretory IgA Levels and IBS
There are many inflammatory markers in the body. SIgA, secretory immunoglobulin A, is the most abundant and primary antibody response in mucosal linings such as the gut lining. It is crucial in preventing bacterial overgrowth and infection. Low levels of SIgA are associated with dysbiosis and infection as well as present an increased risk of IBS among other gut issues. Over 70% of our immune function comes from the gut and the gut microbiota. This is an important reason why getting adequate and appropriate testing done is crucial.
Since low levels of SIgA are associated with IBS, those affected are at higher risk for infections such as H. Pylori, candida/yeast overgrowth, parasites, and other bacterial infections.
Symptoms of H. Pylori infection are similar to that of IBS which is why it can often go undetected for a long time, yet another reason why testing is crucial.
Triggers – Identifying the Common Triggers of IBS
There are many triggers to IBS. Common triggers include trigger foods like refined grains, gluten, processed foods, undigested proteins, caffeine and carbonated drinks, dairy, toxins, FODMAPS (types of sugars), stress & anxiety, drugs, and even menstruation.
It is important to note that triggers are not necessarily root causes. Your gut issues may be progressing towards healing and symbiosis but then a trigger causes a flare in symptoms. This is why identifying triggers and avoiding them is important in the healing process.
While a lot of these triggers vary from person to person, it is important to narrow it down through testing, trial and error, and elimination to find your triggers and trigger foods and ultimately eliminate them. Working with a functional medicine dietitian to go over potential trigger foods and work through an elimination diet to eliminate them is key in managing IBS symptoms and preventing a flare-up.
Certain environmental risk factors such as toxins like glyphosate can also impact and trigger IBS symptoms. Glyphosate is an herbicide used to kill weeds that may be present in foods containing wheat and ultra-processed vegan products like Beyond Burgers.
Other modifiable risk factors for IBS include sleep (and making sure you’re getting adequate amounts of it), maintaining proper hydration, and limiting stress.
Can Smoking Cause IBS Symptoms?
While smoking has many negative effects on overall health, it can also be a contributing factor to IBS. Smoking throws off the bacteria in the gut and can alter the gut microbiome which can trigger IBS. Smoking also can cause an increase in heartburn and acid reflux IBS symptoms as well. Nicotine from smoking acts as a vasoconstrictor meaning it tightens blood vessels which can create a stress response in the body and as mentioned previously, can result in increased IBS symptoms.
Other factors that can flare up or cause IBS symptoms include eating too quickly/not mindfully, not chewing your food properly, certain medications like antibiotics as well as regular use of over-the-counter NSAIDs like Advil, Tylenol, etc. which alter the gut microbiome, and toxins like environmental toxins, heavy metals, glyphosates, and plastics such as those that we may be cooking with.
Mental health plays a role in triggering IBS symptoms as well. Your neurological system and your gut are intertwined, this is known as the Gut-Brain Axis. As changes in mental health occur, the brain releases different chemicals throughout the body depending on the mental changes. When we feel anxious, the brain releases stress hormones/chemicals to the gut which can result in abdominal pain, changes in gut bacteria, and other IBS symptoms. Another important thing to mention is that certain neurotransmitters such as serotonin actually have higher quantities in the gut than in the brain. Gut dysbiosis can affect serotonin regulation and result in surges and hypervisceral sensitivity.
Hormonal changes like those listed above are not the only kinds that can trigger IBS symptoms. For women, changes in hormones or fluctuations in hormones that occur within the monthly menstruation cycle can also be triggers for IBS symptoms. To simplify it, there are receptor cells for female hormones (the same hormones that fluctuate depending on where in the cycle you are) in the GI tract. As estrogen and progesterone change throughout the cycle, it can impact GI function and thus cause a trigger in IBS symptoms.
Most commonly, women may see that their IBS symptoms are worse during menstruation. These same hormones are also what help control the muscular contractions of the intestines which control how quickly food is able to travel through the GI tract. Understanding your cycle and knowing where you are in your cycle is crucial to knowing how and what to eat to decrease these triggered symptoms.
Hidden Risk Factors for IBS
Genetics and family history also play a huge role. While IBS is not always a result of genetics and while some of the genes associated with IBS are polygenic, meaning there is more than one genetic variant associated with IBS, those with a family/genetic history of IBS have up to a 57% likelihood of also having IBS symptoms in their life. The polygenic genetic variants associated with IBS are also unique in that environmental triggers can cause them to activate and flare up IBS symptoms.
Test, Don’t Guess…IBS Functional Medicine
Uncover the Root Cause of Your IBS with Professional Support!
What is the root cause of IBS? While listening to your body can tell you so much, functional lab testing is the best way to identify gaps in health and understand where we may need more support. The following functional nutrition tests are crucial in evaluating all parts of the human body that can be affected by or can affect IBS.
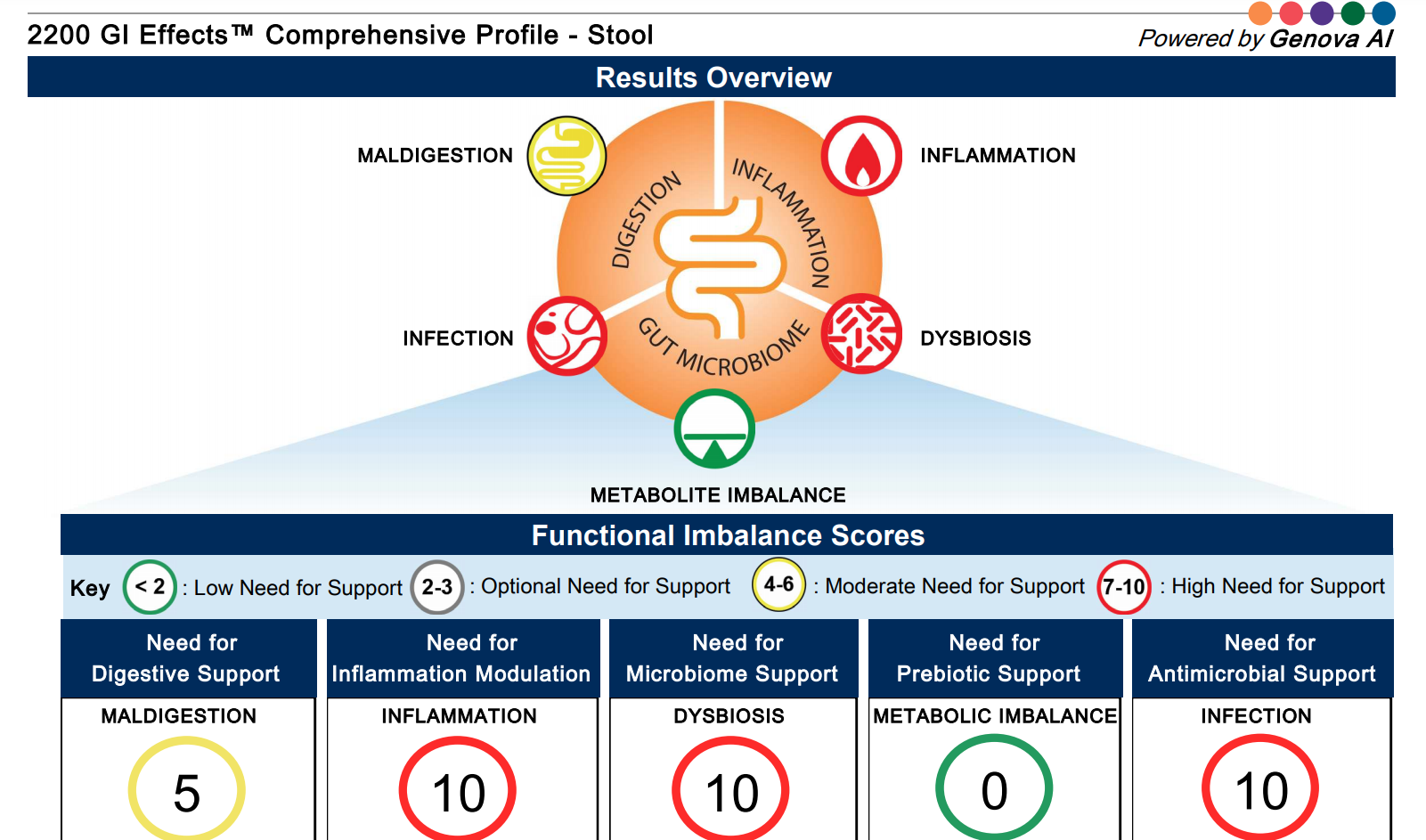
GI Effects: The GI effects comprehensive stool test helps us look at your digestive health and how it is affecting your gut microbiome, inflammatory markers, immune markers, and infections, all of which translate to tell us about your gut health status. Specifically, we are looking for signs of gut dysbiosis through things like candida, parasites, enzyme deficiencies, and more.
The GI effects comprehensive profile gives us a baseline of so many things that can be indicative of root causes, triggers, and more. The Genova comprehensive digestive stool analysis is one of the first things we will look at to begin to understand and tackle the root causes of gut problems.
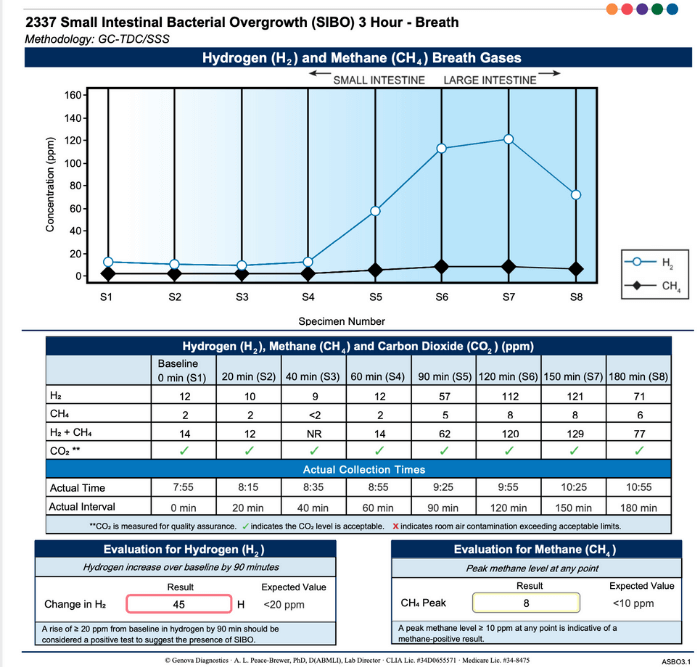
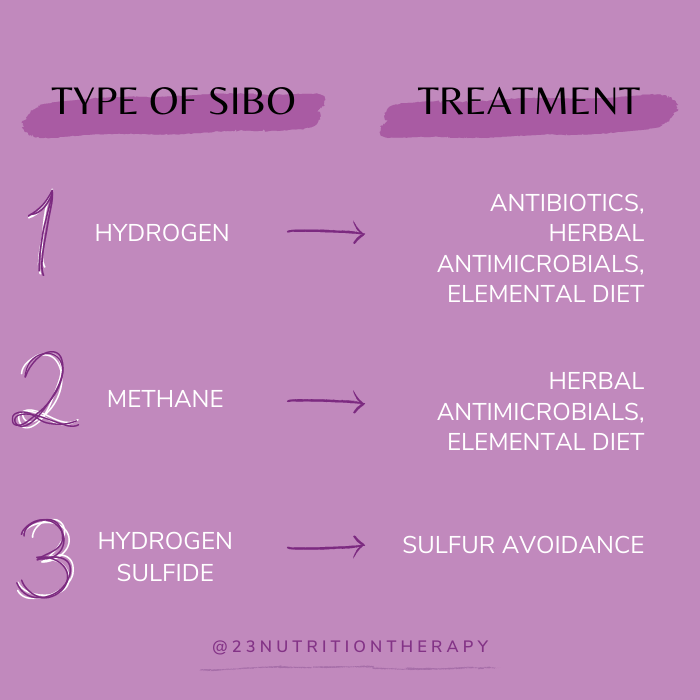
SIBO Test: The small intestine bacterial overgrowth or SIBO test is not a primary test we run. SIBO is generally not a root cause but rather a secondary issue thus targeting it may clear the SIBO but it will come back as the root cause is still unknown. SIBO can also affect/cause underlying motility issues. Instead, we look to clear the imbalances identified from the stool test first and find the root cause to prevent SIBO recurrence. Once all other avenues have been exhausted, we will run a SIBO test to monitor progress.
The Adrenocortex Stress Profile: The adrenal test looks at specific hormones produced by the adrenal system such as cortisol and DHEA which are altered by stress and can be inflammatory markers. Imbalanced adrenal hormones can affect the gut and gut barrier which can result in increased digestive symptoms. Overall this test helps identify the best treatment for adrenal burnout recovery.
ION: The Individualized Optimal Nutrition test (blood and urine) measures organic acids, fatty acids, and amino acids as well as heavy metals and micronutrients. Organic Acids are intermediates or by-products that are produced by the body during a detox, energy synthesis, and more. This test helps us look deeper at oxidative damage, blockage of detoxification pathways, and markers for bacterial overgrowth.
The ION profile presents an amino acid profile containing your levels of essential and non-essential amino acids and their assessment of the levels, homocysteine levels which are an important marker for methylation and cardiovascular disease. It also includes a panel specifically to assess toxic and heavy metals in the body.
The coenzyme Q10 panel included in this test measures the levels of vitamins specifically involved in antioxidant function and oxidation markers which help us understand the level of oxidative damage to membranes in the body. The fatty acid profile assesses omega 3 and omega 6 status which is crucial for inflammation. The ION test also looks at minerals such as RBC magnesium, zinc, selenium, copper, potassium, and calcium.
3×4 Genetics: This test results in a full genetic blueprint. Once we get this blueprint, we are able to look for different mutations and markers that when combined with your medical and family history, lifestyle, and other test results help us understand where certain issues may be arising from and how to mediate them. Another important thing that we are able to see from the 3×4 Genetics test is metabolic pathways, not just single mutations/markers. We are also able to compare biomarkers with previous labs.
Celiac Non-celiac Gluten Sensitivity Test: This Profile is a blood test that looks at immunologic biomarkers to diagnose Celiac Disease. It is important to note however, that IgG/IgA is only positive in about half of patients with gluten sensitivity thus, clinical correlations such as autoimmune history, IBD, diabetes, etc.. are also necessary in this diagnostic process.
It is also important to note that celiac disease is a genetic disease thus there is a genetic correlation. You cannot test positive for celiac disease without at least one of the six genetic markers; however, you may still test positive for the non-celiac markers.
Discover Functional Medicine Solutions for IBS…Book a Discovery Call!
Irritable bowel syndrome is a complex disorder with many complex treatment strategies. Because of this, many times we may feel overwhelmed or stuck in trying to alleviate symptoms on our own. Getting professional support and working with an expert dietitian may be the next step in your IBS health and gut healing journey. Are you ready to find the root cause of your IBS and change your life? Schedule a free nutrition strategy call and get started today.








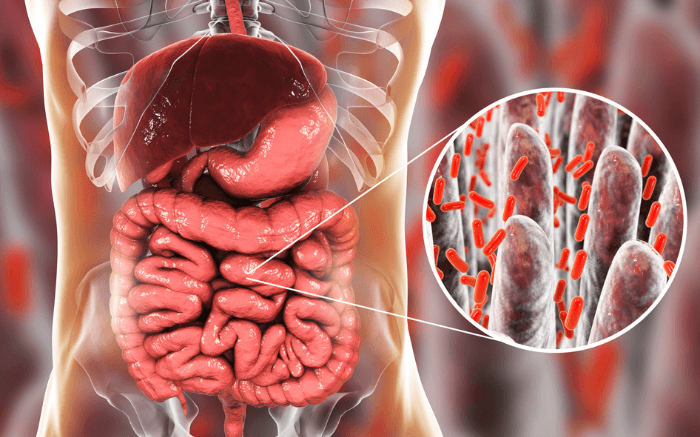
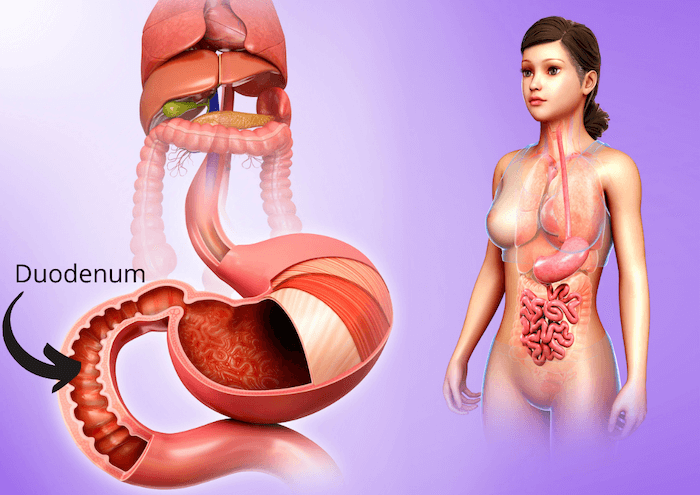
 Increased intestinal permeability becomes an issue when this barrier is compromised and unable to identify or properly separate unwanted substances from the essential nutrients the body needs. When you have a leaky gut, a partially digested protein, allergen, or pathogen can enter the bloodstream. The body will then elicit a natural response better known as inflammation, which in turn causes a further breakdown of the GI tract and a list of symptoms to follow.
Increased intestinal permeability becomes an issue when this barrier is compromised and unable to identify or properly separate unwanted substances from the essential nutrients the body needs. When you have a leaky gut, a partially digested protein, allergen, or pathogen can enter the bloodstream. The body will then elicit a natural response better known as inflammation, which in turn causes a further breakdown of the GI tract and a list of symptoms to follow. 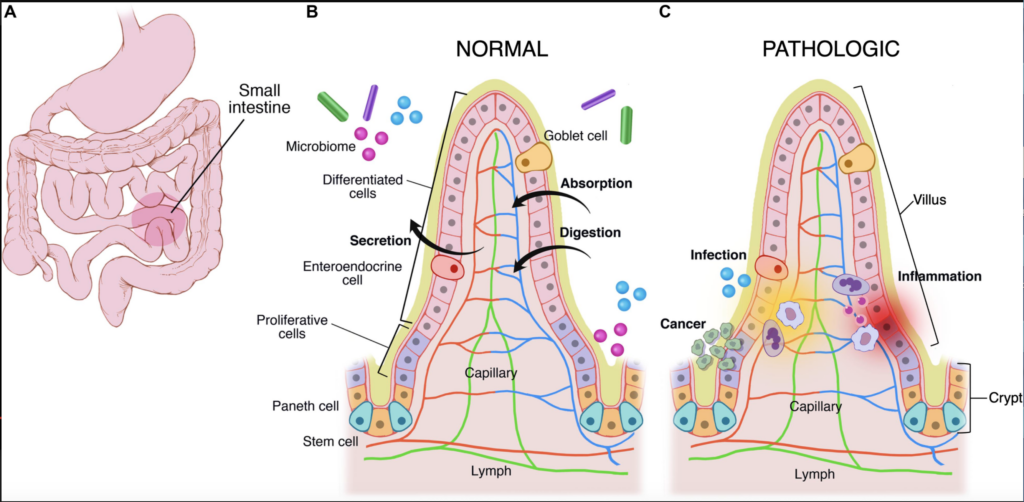 Leaky gut happens when inflammation breaks down the gut lining tissue to make sugar for the blood stream, essentially shredding the gut lining. Now, rather than acting as a selective barrier, the lining becomes more like a sieve. During this process the villi in the intestine become damaged and are now unable to properly absorb fat soluble nutrients. Essential fatty acids, vitamin D, vitamin E, vitamin A, and vitamin K are the main fat-soluble nutrients. They all play integral roles in a multitude of processes in the body. As villi are being destroyed, crypts within the gut lining deepen, hiding parasites and making them difficult to find and treat.
Leaky gut happens when inflammation breaks down the gut lining tissue to make sugar for the blood stream, essentially shredding the gut lining. Now, rather than acting as a selective barrier, the lining becomes more like a sieve. During this process the villi in the intestine become damaged and are now unable to properly absorb fat soluble nutrients. Essential fatty acids, vitamin D, vitamin E, vitamin A, and vitamin K are the main fat-soluble nutrients. They all play integral roles in a multitude of processes in the body. As villi are being destroyed, crypts within the gut lining deepen, hiding parasites and making them difficult to find and treat.  If you suspect you may have leaky gut, consider a stool test to identify any pathogen invasions. After a pathogen killing program, you can begin the healing process by adding more gut-friendly foods to your diet.
If you suspect you may have leaky gut, consider a stool test to identify any pathogen invasions. After a pathogen killing program, you can begin the healing process by adding more gut-friendly foods to your diet.